In the spring of 2000, in Manchester, N.H., a two-year-old Sudanese girl named Sunday Abek, just three weeks removed from an Egyptian refugee camp, was treated at an emergency room for a low-grade fever and vomiting. A throat culture turned up positive for strep, and she was sent home with an antibiotic prescription. Three weeks later, as her vomiting worsened, Abek was admitted to the hospital; there, she fell into a sudden coma. By the time her doctors properly diagnosed her, it was too late. Cause of death: acute lead poisoning.

Lead astray.
Photo: U.S. EPA.
In one sense, the shock that attends this story is testament to a remarkable environmental health achievement: There has been only one other documented case of fatal childhood lead poisoning in the U.S. since a 1978 ban on the residential use of leaded paint. In the 1950s and 1960s, by contrast, acute lead poisoning was a fairly routine cause of pediatric hospital admissions; during a three-year period in the 1950s, for example, there were 94 fatal cases in New York City, Cincinnati, St. Louis, and Baltimore alone.
But in another sense, the Sunday Abek tragedy highlights the limitations of our current approach to lead-poisoning prevention. The source of Abek’s fatal dose was not the Egyptian refugee camp that her family had just left, but the New Hampshire apartment where they sought sanctuary. Abek’s favorite play spots were the porch and the area around the living room windows. That porch, it turns out, was a mess of peeling, flaking, leaded paint — 35 percent pure lead, more than 500 times the safe level — and that window well contained more than eight times the safe amount of lead-contaminated dust.
Those conditions — deteriorated leaded paint and elevated levels of lead-contaminated house dust — are found in 4.4 million U.S. homes with young children. As a result, there are almost half a million lead-poisoned children in the U.S. In the Northeast’s urban core, where a high percentage of housing was built when the concentration of lead in paint was at its peak (before 1950), the problem is especially dramatic. At its worst, it is an epidemic: In Providence, R.I., 20 percent of children who entered kindergarten in 2003 had been lead-poisoned.
Wrap your head around that number: 20 percent … one in five … six kindergartners in a class of 30. To be sure, these kids are not at risk of death (Abek’s blood lead level was a stratospheric 30 times higher than that of most of the kindergartners), but the dangers of lower-level, clinically asymptomatic lead poisoning can be crushing and lifelong: diminished learning capacity, radical behavioral changes (attention deficit disorder and hyperactivity, for instance), and, ultimately, limited job prospects.
Who is responsible for the harm caused these children? And why, more than 25 years after the leaded paint ban, are children still exposed to dangerous levels of leaded paint and lead-contaminated dust? Why has the task of preventing a disease that is invariably referred to as “entirely preventable” proved so maddening?
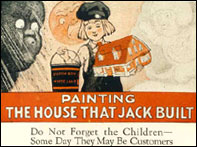
A 1920s lead-paint ad targeted at paint dealers.
Photo: Cincinnati Children’s Hospital.
The first documented case of childhood lead poisoning in the U.S. was in 1914. By 1930, leaded paint was regulated or banned in most European countries. Alas, in the U.S., it was a different story altogether. As detailed by public-health professors Gerald Markowitz and David Rosner in their book Deceit and Denial, the U.S. lead industry’s response to the growing evidence of the harmful effects of leaded paint was to launch a massive, multi-decade advertising campaign in popular magazines — much of it in the form of pictures and rhymes targeted directly at children — that emphasized the beauty, safety, and durability of lead paint for interior use in nurseries, schools, and hospitals. After 1950, the industry consistently fought potentially hard-hitting federal and local regulation of its products.
Malevolent behavior, to be sure, but at least as much to blame for children’s exposure today is policy makers’ failure to heed the lesson of the 1978 leaded paint ban: lead poisoning is fundamentally an environmental, not a medical, problem. In pursuing a strategy that focuses on diagnosing poisoned children (the effect) rather than identifying toxic houses (the cause), we have guaranteed that children will continue to be poisoned for years to come. We must break this cycle by directing resources toward identifying toxic houses before they poison children

Time to get the lead out.
Photo: U.S. EPA.
And when we identify these houses, we must require a permanent remedy: the complete removal of all leaded paint. The primary reason that regulatory authorities condone less strict remedies is cost: The price of permanent abatement ranges from $5,000 to $10,000 per housing unit. But any halfway, so-called “lead-safe” standard that requires only the “cleaning and covering” of leaded surfaces will, in the long term, be neither safe nor cost-effective. As Dr. John F. Rosen, founder of the Children’s Hospital at Montefiore’s Safe House for Lead Poisoning Prevention, and his colleague Paul Mushak wrote in 2001, “Lead-painted surfaces in good condition rarely remain so. What was once intact lead-based paint is the source of all lead-bearing dust and paint chips. Therefore, it is the presence of lead paint on surfaces that defines the hazard, not the condition of surfaces containing lead paint.”
But where, in these times of federal and state belt-tightening, will the funding come from for this massive environmental clean-up? If the state of Rhode Island has its way, the former manufacturers of leaded paint, which for years profited from a reckless disregard for children’s health, will foot the bill. This April, the state will retry its first-in-the-nation public-nuisance lawsuit against the manufacturers (the first trial ended in a hung jury in 2002). Should Rhode Island emerge victorious, other states will surely get in line for a slice of a very large pie. And perhaps Sunday Abek will not have died in vain.
— The editors


