Many of us have spent the last two-and-a-half years worried about the health risks posed by other people. In the United States alone, more than 1 million have died from COVID-19, a painful consequence of how ill-prepared the nation was (and, in many ways, still is) for an infectious disease outbreak.
As the climate warms, more health risks will come not only from other people, but increasingly from the environment around us. We’re equally unprepared to handle those.
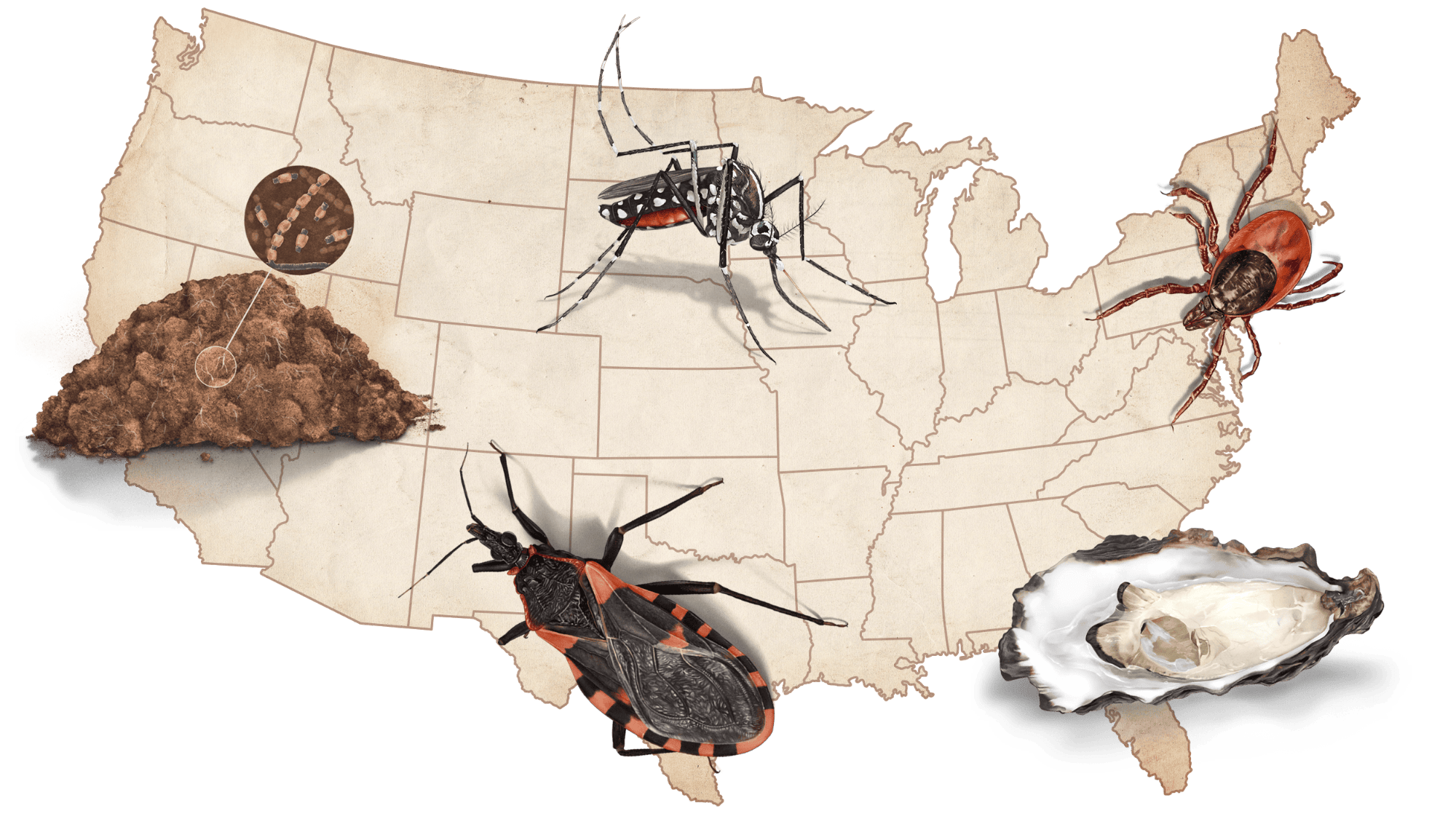
Some of these risks come from diseases that many of us are already familiar with: Lyme disease, for example, which is carried by ticks, or West Nile virus, proliferated by mosquitoes — both vector-borne diseases spread by blood-sucking arachnids and insects. But the environment harbors dozens of other carriers of illnesses you’ve probably never heard of. They come from bugs, shellfish, and even soil. With global temperatures rising, well-known vector-borne illnesses are becoming more common, and other, lesser-known diseases are spreading into new areas.
These illnesses will “continue to tax our public health and medical care systems for years to come,” experts from the Centers for Disease Control and Prevention, or CDC, wrote in a 2016 analysis. “The question remains whether we will be prepared.”
This field guide to tomorrow’s climate-driven diseases introduces you to some of the carriers that are growing in number and expanding into new parts of the U.S. as the environment changes. The viruses, bacteria, fungi, and parasites they spread can cause joint pain, skin lesions, long-term memory problems — even death. Some of these maladies have no treatment or cure, though experts emphasize that numerous preventative measures to limit infection exist. In other cases, successful treatment depends on a rapid diagnosis by a medical professional, but doctors in areas where disease carriers have historically been rare are struggling to recognize an onslaught of unfamiliar illnesses. Ensuring a less deadly future requires taking actions right now to protect ourselves against what’s coming. The first step, as with any climate change-related issue, is sizing up the scope of the threat.
Powassan virus
Carried by the blacklegged (deer) tick, an arachnid about the size of a poppy seed
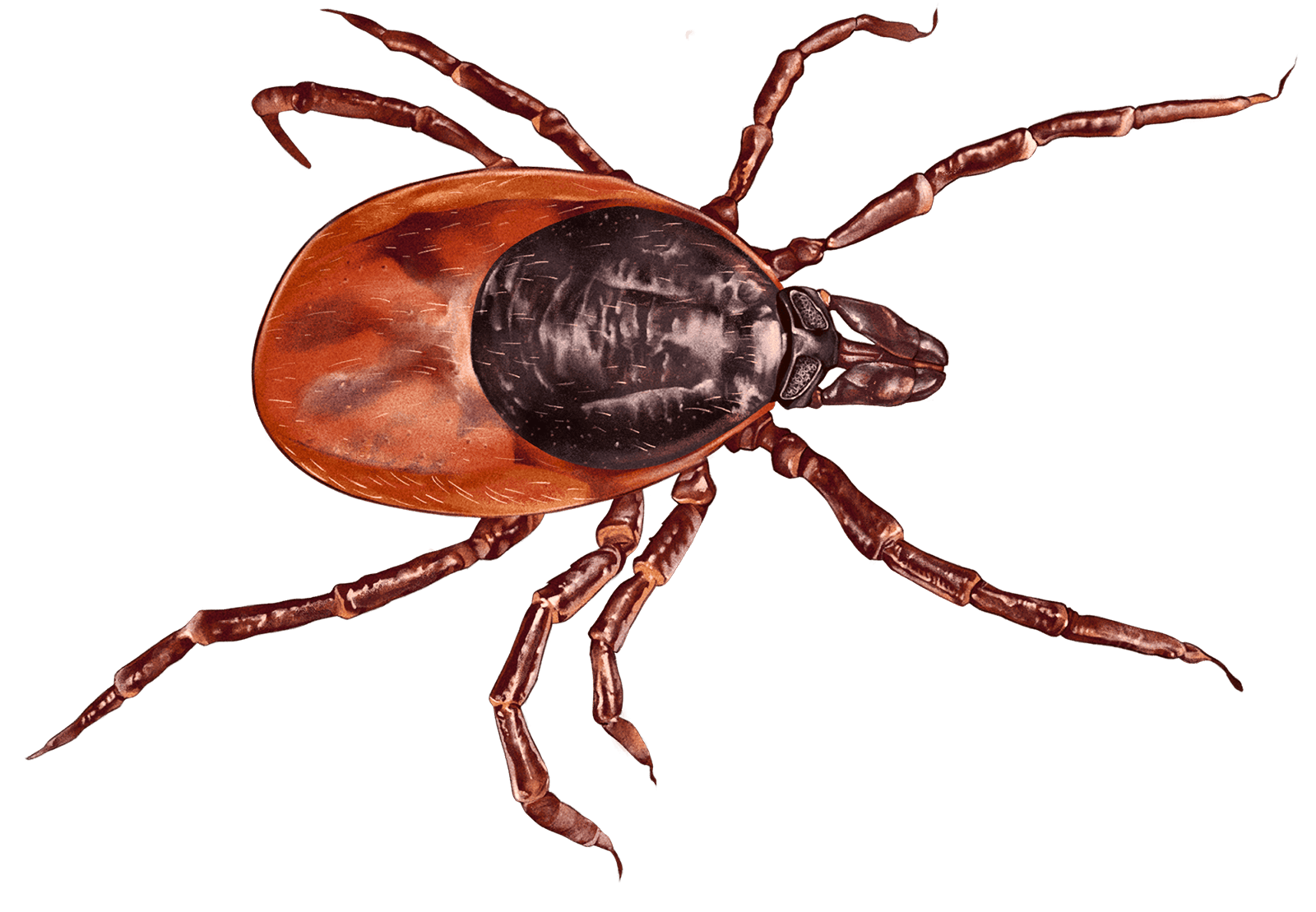
Powassan virus, or POWV, is a rare, tick-borne illness that infected just 134 people in the U.S. between 2016 and 2020. That may not sound like a lot, but it represents a more than 300 percent increase from the previous five-year period.
The virus causes a neuroinvasive disease that has no treatment, vaccine, or cure. Early symptoms include headache, fever, nausea, and weakness — similar to other tick-borne illnesses. But Powassan is different from most tick diseases because it has an extremely high mortality rate: One in 10 people who develop the acute form of the illness die. Half of those who survive a severe bout of Powassan have long-term health issues such as recurring headaches, loss of muscle mass and strength, and memory problems.
In May, an elderly woman in Connecticut died weeks after contracting the Powassan virus, the second fatality caused by the illness in the U.S. this year.
Powassan virus has mainly been found around the Great Lakes and in the Northeast, but, between 2016 and 2020, cases were reported as far away from those regions as North Dakota and North Carolina.
Historically, the range of blacklegged ticks has been constrained by environmental factors — ticks can’t survive winters that are very cold or conditions that are too dry. But changing weather patterns and warming temperatures have allowed this tick to grow in number and expand its hunting range into new territories, catching people and the doctors who treat them off guard.
“Roughly 50 percent of those who recover from an acute Powassan infection have some kind of long-lasting, if not permanent, debilitation.”
While there is no vaccine or cure available for people who contract Powassan virus, researchers at Yale University are working on an mRNA vaccine that could help protect against many tick-borne illnesses at once. The vaccine targets ticks by making it harder for the bloodsuckers to extract a full blood meal from animals, and hopefully one day humans, once they latch on. Until vaccines such as this one are widely available, the best way to avoid a tick-borne illness is to exercise extra caution in areas where ticks are common, use insecticides such as permethrin on the hems of your pants, and check your body for ticks regularly.
Chikungunya fever
Carried by Aedes aegypti and Aedes albopictus mosquitoes
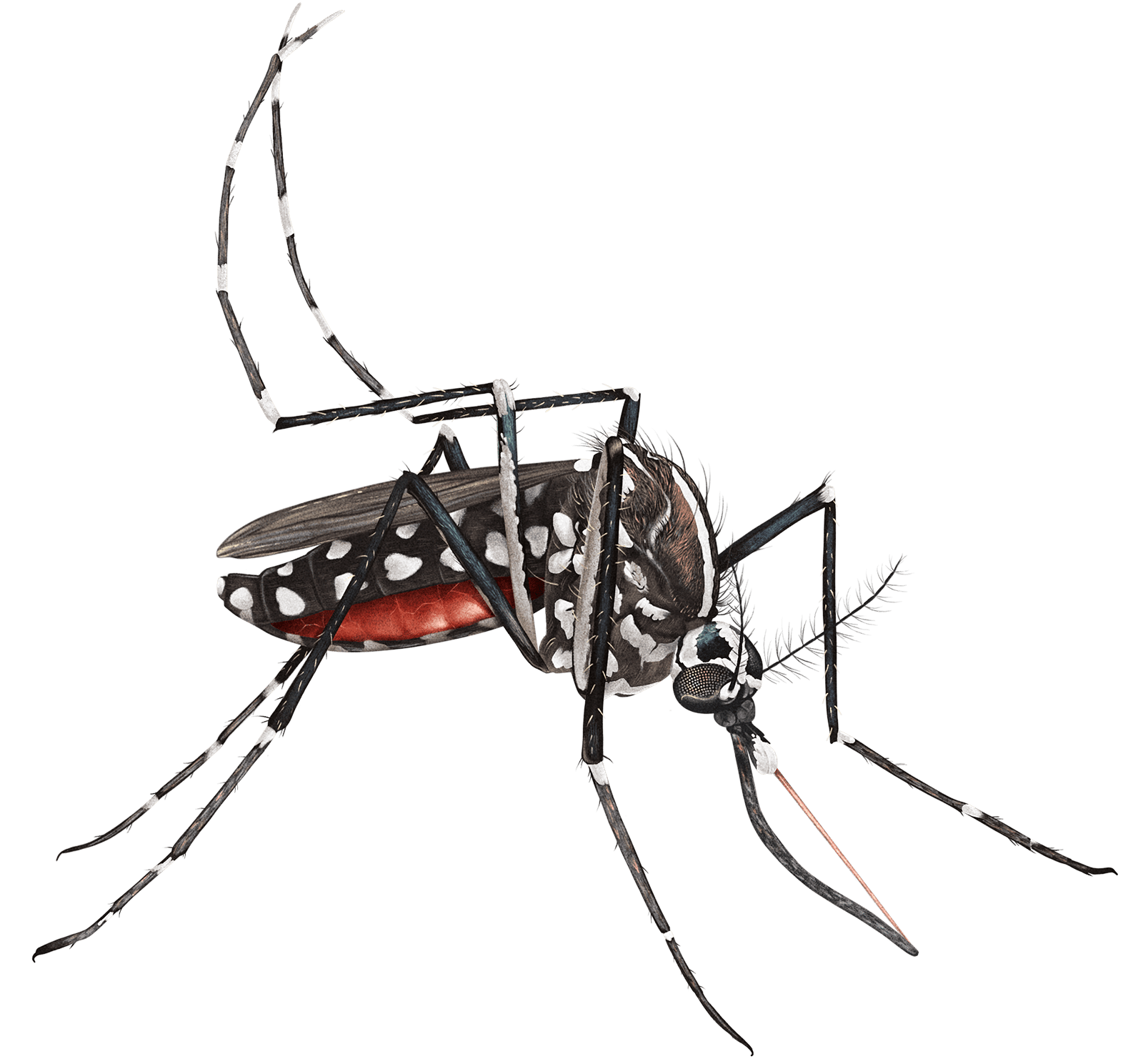
The virus that causes chikungunya is still rare in the U.S., but experts at the CDC are watching it extremely closely because the illness has the potential to spread at blinding speeds. The first case of chikungunya in the Western Hemisphere was discovered in 2013 in the Caribbean. By 2014, it had become an epidemic in Jamaica, and an outbreak of 107 cases had been documented in Florida. By 2017, more than 1 million people had been infected in the Americas. Some 80 percent of the Jamaican population may have been infected.
Symptoms include fever, debilitating joint pain, muscle pain, headache, nausea, fatigue, and rash. Death from chikungunya is rare and mostly occurs in severely immunocompromised patients. Severe joint pain can persist for months and even years in some cases.
Chikungunya fever was first identified in Tanzania in the 1950s, remained relatively rare for half a century, and then exploded into more than 60 countries throughout Asia, Africa, Europe, and the Americas after 2004. Since 2014, cases of the virus in the U.S. have been identified in Florida, Texas, Puerto Rico, and the U.S. Virgin Islands. Most of those cases were acquired after travel to countries where chikungunya is more prevalent.
Much like ticks, mosquitoes thrive in warm, moist conditions. Climate change isn’t just warming the planet, it’s throwing the hydrological cycle out of whack, causing periods of extreme wetness in regions all over the globe. These conditions may be encouraging the spread of the mosquito species that carry chikungunya from California down through the southern half of the U.S. and up into the Northeast.
“We are not prepared.”
Similar to Powassan virus, chikungunya has no vaccine or cure. Doctors can make patients more comfortable with fluids, local anesthetics, and aspirin. The most effective tools against chikungunya are preventative. To that end, the Environmental Protection Agency recently approved the release in California and Florida of 2.4 billion genetically modified Aedes aegypti mosquitoes that have been engineered to only produce male offspring. The initiative is aimed at reducing the number of female mosquitoes — the only ones that bite — in the environment. By shifting the gender balance, it could also eventually lead to a reduction in the number of these insects buzzing around in the U.S.
Vibriosis
Carried by uncooked shellfish such as clams, mussels, and oysters

Vibrio is a marine bacterium that lives in the salt and brackish waters of estuaries around the globe. Different strains of Vibrio can cause infections of varying severity. Vibrio vulnificus is a particularly dangerous variant.
Shellfish can accumulate high concentrations of Vibrio and then pass that dose on to humans if consumed raw. Humans can also be infected with Vibrio when swimming in water with an open wound. When it infects humans via an open wound, Vibrio vulnificus can end up causing necrotizing fasciitis, or flesh-eating disease. If the bacteria is ingested orally, it enters the bloodstream and can cause large pus-filled lesions on the extremities. The chance of death following a wound-acquired Vibrio vulnificus infection is 25 percent. That number doubles with food-borne infections. Immunocompromised people are particularly at risk.
Vibrio vulnificus is found in the Gulf of Mexico and, more recently, along much of the East and West Coasts.
The optimal water temperature for all Vibrio, including Vibrio vulnificus, is between 68 and 95 degrees Fahrenheit. Coastal waters around large swaths of the U.S. are hitting that temperature threshold earlier in the year as the planet warms, giving Vibrio a longer window to proliferate in the water and potentially accumulate in shellfish. In addition, water that has historically been too chilly for Vibrio vulnificus to properly thrive is warming up, allowing the bacteria to spread north into new areas like the Northeast and Pacific Northwest, and even into Canada.
“If you feel bad when you go to bed, by the time you wake up you could be ready for amputation, so don’t sleep on it. Go to the doctor as soon as you feel ill.”
Pay attention to signage and advisories from your local public health department when harvesting your own shellfish. Cook your bivalves thoroughly before eating them, or be careful not to leave shellfish out in the sun or in a warm place if you plan to eat them raw. And never swim with an open wound, even if the injury is very small.
Antibiotics can knock out vibriosis, but only if they’re administered early in the infection.
Chagas’ disease
Carried by triatomine insects, commonly known as kissing bugs

Kissing bugs are bloodsucking insects that often attach themselves to the soft skin around the mouths of humans, dogs, and other animals. But Chagas isn’t spread by the bloodsucking itself. When kissing bugs feed — at night when people are sleeping — the bugs defecate. People tend to rub the kissing bug’s feces into their mouths by accident either in their sleep or when they wake, inadvertently infecting themselves with Trypanosoma cruzi, the parasite that causes Chagas.
In the weeks and months after infection, symptoms can include fever or swelling. If Chagas is left untreated, it becomes chronic. An estimated 20 to 30 percent of people with chronic Chagas develop life-threatening complications such as a dilated heart that can’t pump enough blood, life-threatening gastrointestinal issues, and cardiac arrest.
Millions of people in the Americas have been infected with Chagas since the first human case of the disease was diagnosed in 1909 in Brazil. Some 300,000 of them live in the United States, but most live in Latin America. A vast majority of the Chagas cases documented in the U.S. have been in immigrants who came to the country from Latin America or elsewhere where the parasite is prevalent.
While Chagas is still relatively rare in the U.S., climate change could help the disease spread by causing an increase in the number of triatomine insects across the nation. Kissing bugs have already been found in 29 U.S. states, and researchers have documented the Chagas parasite in 55 percent of those bugs. Research shows the temperature increases expected under climate change will cause kissing bugs to mature faster and bear more offspring, which suggests that cases of Chagas may rise as the planet warms.
“[Chagas’ disease] is already in the U.S. but spreading and will become a big problem.”
Chagas can be knocked out by antiparasitic medications if it’s caught early. Chronic Chagas can also be treated with similar medications, but success is less certain. In the U.S., six states currently screen blood donations for evidence of the parasite. However, only four of those states require that cases be reported to public health authorities, so it’s difficult for the CDC to ascertain how many cases of Chagas there are in the U.S. and how quickly they are rising. Window screens and insecticides may help control the insect when it becomes more widespread in the U.S.
Valley fever
Carried by soil containing the fungus Coccidioides
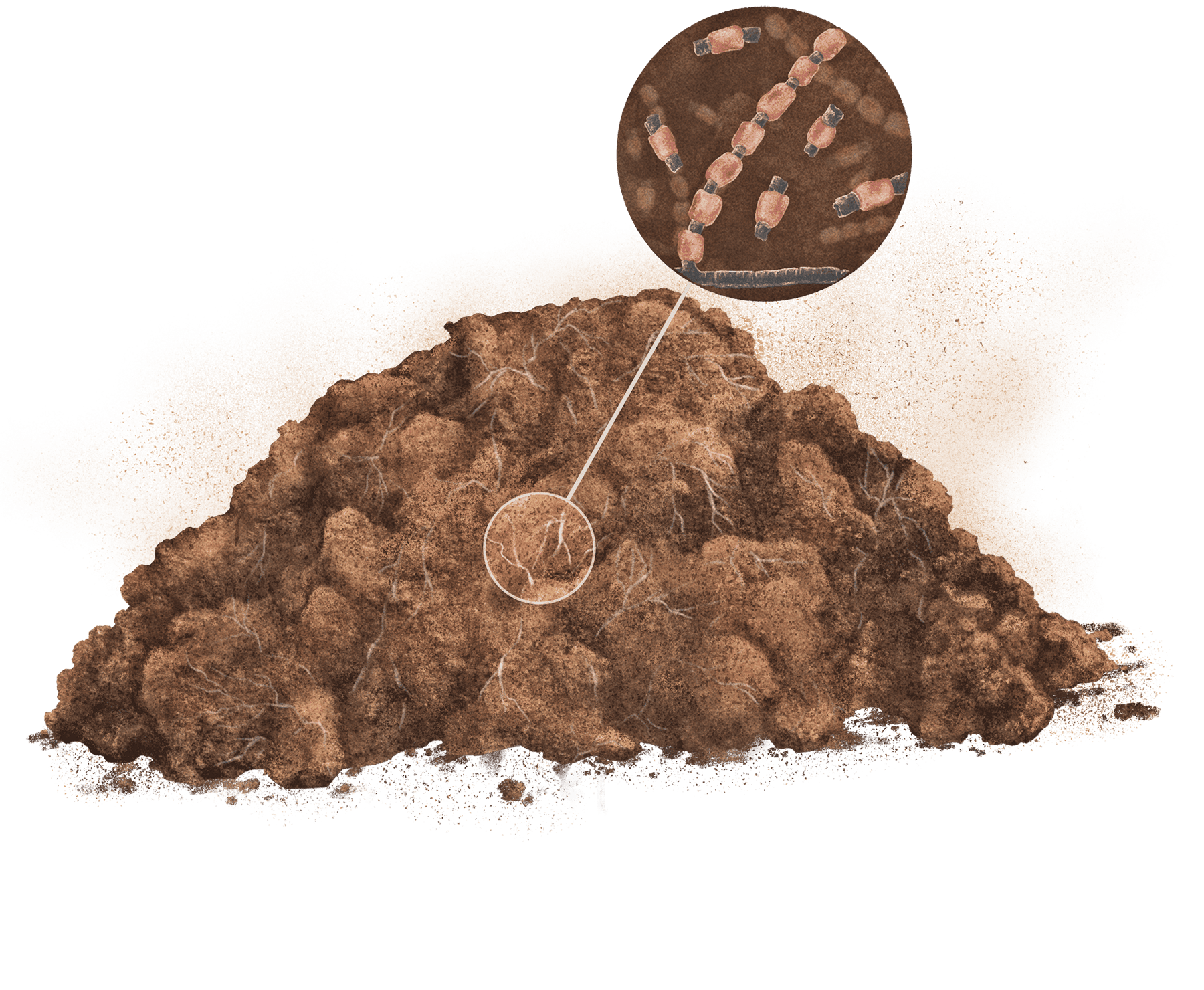
When Coccidioides spores living in dirt circulate in the air — kicked up by wind, construction, farming, or possibly wildfire smoke — humans and other animals can breathe the spores in. Most individuals with healthy immune systems can fight off the fungus by themselves, but in people with compromised immune systems, the spores are more likely to survive and extend their fungal filaments throughout the lungs and sometimes the rest of the body. Studies have also shown that pregnant people, Filipinos, African Americans, and perhaps Native Americans are more prone to hospitalization after contracting the disease than other demographics, even if they have healthy immune systems.
Some 60 percent of Valley fever cases produce no symptoms or mild symptoms that most patients confuse with the flu or a common cold, including fever, headache, and fatigue. But 30 percent of those infected develop a moderate illness that requires medical care. And another 10 percent have severe infections — when the fungus spreads beyond the lungs into other parts of the body. Those cases cause meningitis and can be fatal.
Valley fever has been documented in the desert Southwest and parts of California for decades. Cases have cropped up recently in the Pacific Northwest and non-desert areas in the Southwest. Arizona has the highest rates of Valley fever in the U.S. The disease is also prevalent in Mexico and Central and South America.
The fungus that causes Valley fever thrives in warm, wet conditions. Researchers have demonstrated that, if the world continues emitting greenhouse gases, much of the U.S. could become hospitable to the fungus. Cases are already on the rise. Valley fever cases in the U.S. rose by 32 percent between 2016 and 2018, according to the CDC. One study determined that cases in California rose 800 percent between 2000 and 2018. Oscillating drought and flooding in certain areas, a cycle research shows is exacerbated by climate change, could lead to even more cases. Like most other fungi, Coccidioides proliferates after heavy rain. When drought hits after the rainy season, those rain-fueled spores can get kicked up out of the soil and settle in people’s lungs.
“In terms of how severe it is and the lifelong requirement for some of these people for treatment, it’s worrisome. It would be a bad thing to see more Cocci than we have already.”
Caught early, Valley fever can be beaten back with antifungal medications. But the problem is that doctors in states where the disease is not common may not know Valley fever’s warning signs. If diagnosis is delayed, the more severe forms of the illness are more difficult to treat and can result in death; antifungal treatments are not a cure and can only give your immune system a boost as it works to fight off the fungus. Researchers in Arizona are working on a vaccine against Valley fever for dogs. At some point in the future, with enough funding, the researchers hope they can apply the same vaccine research to developing an inoculation against the fungus for human beings.
License: ©2022 Grist / PDF: 8.5×11
License: ©2022 Grist / PDF: 11×17
This story was reported and written by Zoya Teirstein. Illustrations were done by Amelia K. Bates. Design and development were handled by the Innovation & Growth team. Art direction by Teresa Chin. Megan Merrigan and Angelica Arinze handled promotion.
The project was edited by Katherine Bagley and L.V. Anderson. It was copy edited by Joseph Winters and fact-checked by Lina Tran.
For a downloadable field guide to emerging climate-charged diseases, click here:
8.5×11 | 11×17