This story was originally published by Mother Jones and is reproduced here as part of the Climate Desk collaboration.
“We should get out of here,” says air pollution chemist Eben Cross. At 7 a.m. on this cold November day the wind blows steadily through the Massachusetts Institute of Technology’s Cambridge campus, cutting through our thin jackets. But Cross isn’t afraid of the cold. He worries about the air we’re breathing — especially considering the six fire trucks directly ahead, idling in the dim morning light.
“We’re getting hammered right now,” Cross says, shouting over the hum of the engines. He’s taken his gloves off to manipulate the display panel on his pollution monitor. The acrid smell of diesel is unmistakable. “Anytime you can smell it, you are in a regime that is very polluted,” he says. “In many ways your nose is a better mass spectrometer than any device on the market.”
Cross’ monitor measures the presence of microscopic particles suspended in the air. Earlier, in his home, the device reported average concentrations of between 10,000 and 100,000 airborne particles per cubic centimeter of air (the latter after he burned some toast). Now it detects millions. The massive size of the fire trucks’ engines, combined with their inefficient combustion in cold weather, means that the air reaching us is replete with fine and ultrafine particles — specks of waste at least 36 times finer than a grain of sand, often riddled with toxic combinations of sulfate, nitrate and ammonium ions, hydrocarbons, and heavy metals. Though we have long known that these tiny particles cause and exacerbate respiratory problems — like asthma and infections and cancers of the lungs — they are also suspected to contribute to a diverse range of disorders, from heart disease to obesity. And now cutting-edge research suggests that these particles play a role in some of humanity’s most terrifying and mysterious illnesses: degenerative brain diseases.
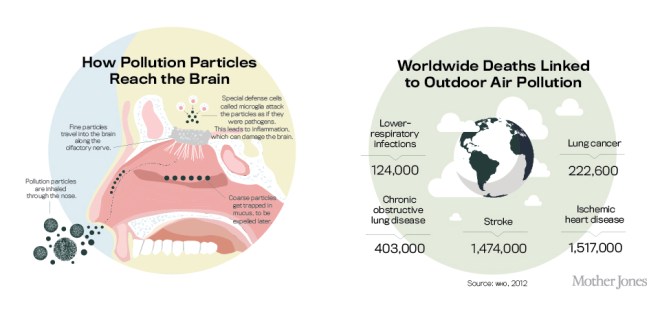
While coarse pollution particles seldom make it past our upper lungs, fine and ultrafine particles can travel from our nostrils along neural pathways directly into our brains. Once there, they can wreak a special havoc that appears to kick off or accelerate the downward spiral of degenerative diseases like Alzheimer’s and Parkinson’s. While much of the research is still preliminary, the findings so far are compelling. Autopsies of the brains of people who lived in highly contaminated areas have turned up traces of pollution and corresponding brain trauma. And among those still living, epidemiologists have recorded elevated rates of brain disease and accelerated mental decline.
All of this is especially scary when you consider how many people are at risk. Alzheimer’s and Parkinson’s already afflict 50 million people worldwide and about 6 million in the United States. In 2015, nearly 1-in-5 Medicare dollars will be spent on Alzheimer’s; this disease and other types of dementia will cost the United States $226 billion. By 2050, experts predict, that cost will rise to $1.1 trillion — the baby boomers are only now entering the phase of life when degenerative diseases usually emerge. Because boomers were born before the improvements of the Clean Air Act, passed in 1970, they likely have had a greater lifetime exposure to air pollution than any other generation before or after them.
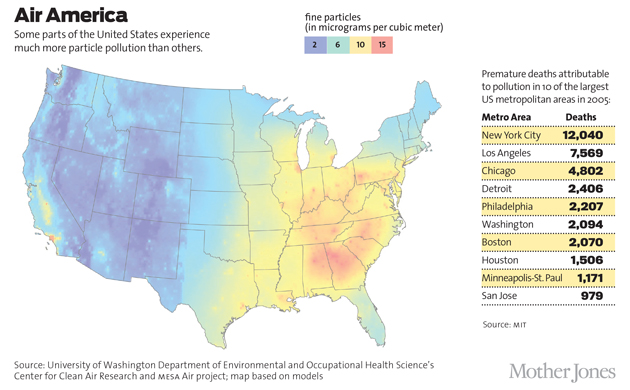
But although American air today is the cleanest it has been in four decades, pollution is still a major public health problem. According to estimates from the American Lung Association, more than 46 million Americans — about 15 percent of the U.S. population — are chronically exposed to levels of particle pollution that exceed Environmental Protection Agency (EPA) standards, with a further 44.1 million plagued by periodic unhealthy exposures on bad air days or, as in parts of California, seasonal air pollution spikes. Meanwhile, in some Chinese and Indian cities, air pollution levels are routinely three to six times higher than World Health Organization standards. A recent study in the peer-reviewed journal Environmental Health and Technology estimated that we could avoid 2 million deaths globally by cleaning up the world’s air.
Researchers have struggled for decades to pinpoint the risk factors that, in addition to genetics, can contribute to a person’s likelihood of developing Alzheimer’s and Parkinson’s diseases; theories have ranged from viral infection to aluminum exposure to high-fat diets, but none of these has withstood scientific scrutiny. The research implicating air pollution is in its early stages, and many questions remain unanswered — for example, it’s unclear whether particle pollution initiates degenerative disease or merely accelerates it. Still, the evidence so far suggests that pollution could be the most pervasive potential cause of brain disease that scientists have ever discovered. We’re not “beyond a doubt,” says Michelle Block, a neurobiologist at the Indiana University School of Medicine, but “everything we do says this is probably happening.”
In a small room on the third floor of a lab at the University of Southern California’s gerontology department, graduate student Nick Woodward shows me one front line in the global effort to understand the link between air pollution and brain disease: nine black mice in clear plastic cages. They are breathing highway exhaust, piped in by Woodward, that was gathered from the busy 110 freeway. Because of the heavy truck traffic on that road, the exhaust is especially rich in ultrafine particles laced with metals and hydrocarbons, in hundreds of combinations. To simulate life in a nearby neighborhood, Woodward explains, the mice will be exposed to exhaust for five hours a day, three days a week, until they are finally sacrificed and their organs examined for the presence of particles and disease.
This study and similar ones have their roots in Mexican research from the 1990s, when the United Nations had just deemed Mexico City one of the most polluted metropolitan areas on the planet. Even modern Beijing sees relatively clear skies 20 percent of the year — but in 1992, Mexico City air quality monitors recorded only eight smog-free days. By the early 2000s, researchers in Mexico City studying the effects of urban pollution on dogs, which live longer than mice and can be raised outdoors to approximate human exposures, began to discover unusual symptoms.
Lilian Calderón-Garcidueñas, lead investigator of the studies, noted that some dogs exposed to Mexico City air began to exhibit “decrements of attention and activity.” Caretakers of other dogs “were aware of alterations of sleep patterns and barking,” she wrote. Some “reported transient episodes during which the dogs failed to recognize [them].” Inside their brains, Calderón-Garcidueñas found dramatic tissue damage — the cells in the dogs’ olfactory-processing center were dying, with the scars of disease traceable out to the nose itself — that was strangely reminiscent of the damage that sometimes appears in an entirely different study population: Alzheimer’s and Parkinson’s patients.
Domesticated dogs have an exquisite sense of smell; they possess as many as 220 million olfactory neurons, while humans are thought to have between 5 million and 12 million. Dogs are also one of only a handful of animal species known to naturally develop Alzheimer’s-type dementia. What Calderón-Garcidueñas discovered more than a decade ago may prove to be the missing element in a long-standing theory of neurodegenerative disease origin. For reasons poorly understood, degenerative diseases like Alzheimer’s and Parkinson’s often reveal themselves in humans through early breakdowns in the olfactory system. Degenerative disease sufferers lose some of their sense of smell so predictably, and so long before more overt symptoms manifest, that doctors sometimes use smell tests as a diagnostic tool. As a result, many neurologists have long suspected that these disorders might be caused by foreign substances that we inhale through our noses. The most recent studies have looked at the most common of these substances: particle pollution.
In order to understand how exactly a particle travels from the nose to the brain, you’ll need a quick lesson in human respiratory anatomy. When you breathe in polluted air, particles enter your body through both your nose and your mouth. Large, coarse particles, like bits of windblown dust, are caught there and in your upper lungs and are eventually removed by coughing, sneezing, and nose running. Smaller particles can bypass these natural defense lines to reach your body’s more sensitive tissue. In the lungs, scientists have long known, they can embed and foster infection and cancer or pass directly into the bloodstream, where they create a host of dangerous byproducts that can circulate with the blood and cause damage to organs and bodily systems.
But particles that make it past your nose may be even more damaging. The lining of the human nasal cavity contains millions of specialized nerve cells that wave tens of millions of tiny hairs in a gel of mucus. These hairs detect inhaled chemicals and transmit information about them to the smell center of your brain, called the olfactory bulb. This is the process that allows you to tell, say, whether a carton of milk is spoiled. Your nasal nerve, whose hairs are exposed to the outside air in your nose, reaches all the way into your brain. This direct line allows your nose to communicate very quickly with your mind, an advantage in hunting, gathering, and predator avoidance. But it also makes us susceptible to pollution — particles entering your nose can actually travel along the olfactory neuron pathways from the nasal hairs right into the brain. In other words, as with cocaine, what you inhale through your nose can go straight to your brain.
Once in the brain, pollutant particles can directly kill or damage neurons if toxic metals or compounds are attached to them. But scientists now know that they can also cause more widespread damage by disrupting microglia, the brain’s unique army of immune cells. Microglia are the sentinels, bodyguards, and trash collectors of the brain. Among other things, they identify threats to brain health, from dead neurons to pathogens, and work collectively to neutralize and remove the offenders. When microglia encounter a pollution particle, they mistake it for a germ — with disastrous results.
Microglia in the presence of a particle produce a variety of chemical compounds meant to kill the interloper. The chemicals then accumulate and begin to damage or even kill surrounding cells. And the toxins attached to particles can corrupt the microglia, leaving them permanently in attack mode or otherwise unable to perform other important functions, like removing waste from the brain.
Researchers believe that chronic inflammation — the long-term overactivation of the body’s immune response — is harmful, even at very low levels. Studies have connected it to a broad range of illnesses; in the skeletal system, for example, it can cause the pain associated with arthritis, while in the gut it can lead to metabolic disorders such as diabetes. In the brain, chronic inflammation has been consistently implicated in neurological degeneration. This is, relatively speaking, old and established science. In scans and autopsies of patients with Alzheimer’s and Parkinson’s, highly active microglia are found in the regions of the brain that have lost the most neurons. And, in mice, scientists have actually observed the microglia killing neurons.
With air pollution, “there is indication that we are creating inflammatory responses that are in the direction of Alzheimer’s disease,” says Caleb Finch, a gerontologist who runs the lab that is studying pollution and mice at USC. If that assessment sounds overly cautious, it’s meant to: Researchers in the Alzheimer’s field are extremely wary of overstating the evidence. Still fresh are the memories of an aluminum scare in the mid-1980s, when preliminary studies linking aluminum in the brain to Alzheimer’s disease fed provocative news headlines and initiated needless hand-wringing over antiperspirants and cooking pans. Also, scientists now increasingly believe that it’s likely that no one environmental factor or trigger causes the disease; rather, “it’s probably a multiple hit,” says Indiana University’s Block. “It’s an assault across your entire lifetime that’s going to culminate with disease in age.”
Even so, of all the potential environmental drivers of degenerative disease, air pollution has by far the most promising scientific evidence behind it. “The longer I’ve been doing this research, the more I’m convinced that, most likely, urban air pollution is the most readily available source of microglial activation,” Block says. Jennifer Ailshire, a social demographer at USC, also sees growing evidence along these lines. It “just hardly ever happens,” she says, that human studies and animal models are in such strong agreement.
In epidemiology, one of the best ways to figure out what leads to a disease is the prospective study, in which scientists track patients over decades, monitoring their diet, lifestyle, exposures to toxins, and health outcomes. Several prospective studies on pollution’s effect on neurodegenerative diseases are underway, but we won’t know their results for decades. What we do have so far are retrospective epidemiological studies, which are kind of the opposite: Scientists study groups of older people with and without a given disease, comparing their life experiences, genetic factors, and environmental exposures. The problem with retrospective studies is that they rely heavily on subjects’ self-reporting, which is notoriously fallible; subjects probably wouldn’t be able to accurately recall, for example, how much time they’ve spent near an idling school bus. Another problem is inconsistent data. For example: Fine-particle levels in the United States have been regularly recorded for only the last 15 years, so epidemiologists often use proxy measures to estimate exposures from the distant past.
Still, evidence from retrospective studies is sobering. Controlling for things like ethnicity, gender, income, education, and other possible environmental exposures (including cigarette smoke), elderly individuals living in areas with polluted air appear to lose their mental abilities faster, show more predementia symptoms (also known as mild cognitive impairment), and develop Alzheimer’s disease at greater rates. Six years ago, researchers in Germany assessed the cognitive abilities of 399 elderly women who lived in the same place for more than 20 years. Regardless of her socioeconomic status, the closer a woman lived to a busy road, the authors reported, the greater the chance that she would have mild cognitive impairment.
Four years ago, researchers from Harvard linked estimates of higher daily exposure to black carbon, a solid type of fine particulate matter, to lower cognitive ability in older men in Boston. In a larger, national study tracking the mental status of more than 19,000 retired nurses over several years, researchers connected the rate of mental decline in women 70 and older to their exposure to coarse- and fine-particle pollution and found that those exposed to more particles lost their mental abilities at a faster rate. In a group of 95,690 elderly Taiwanese, researchers this year found that a slight increase in fine-particle exposure over 10 years led to a 138 percent increased risk of developing Alzheimer’s disease. A smaller, more recent study published in the Annals of Neurology followed 1,403 elderly women without dementia. Scientists found that exposure to air pollution over time to led to a major decrease in the subjects’ white matter, a part of the brain essential for cognition.
So how much pollution might the brain be able to withstand? Unfortunately, that’s not yet clear. In the study from Taiwan, an increase in annual pollution exposure of four micrograms of particles per cubic meter of air — the additional amount you might experience within a block or two from a busy road — was sufficient to dramatically alter Alzheimer’s risk. But that was in addition to already high levels of pollution exposure, which were greater than anything you would routinely experience in America. In the nationwide study of retired U.S. nurses, exposure to an additional 10 micrograms of fine particles per cubic meter of air per year over several years seemed to speed up damage to mental abilities “as if your brain were aged an extra two years,” says Rush University’s Jennifer Weuve, the study’s lead author. That’s about the same increase in pollution you would experience if you moved from Beverly Hills to South Central Los Angeles.
And there is growing evidence that particle pollution’s assault on the mind is not limited to elderly brains. Researchers in Mexico City, which still has some of the worst urban air on the planet, have found signs of advanced brain damage in children as young as 6 and 7 years old: overactive immune cells, degraded white matter, and damaged vasculature typically seen only in older brains. In one autopsy study comparing children raised in Mexico City with their counterparts in less polluted parts of the country, half the Mexico City children had notable aggregations of a protein called amyloid beta — which is strongly associated with Alzheimer’s — grouped in clumps across their brains. In the children from less polluted areas, there were none.
In America, as in most of the world, the burden of pollution does not fall evenly. Fine particles can travel thousands of miles through the air, but ultrafine particles drop out much sooner, typically after only a few thousand feet. This means that unless you live within a few miles of a coal-fired power plant or metal smelter, most of the ultrafine particles you breathe are probably from vehicles, particularly old diesel engines.
In our pass through Cambridge and then Boston, which has average air pollution levels for an American city, Cross detects numerous and dramatic ultrafine-particle pollution hot spots: bike lanes near highways where diesel clouds plague commuters for miles; schoolyards full of emissions from idling buses; apartments downwind of trucking routes. The worst places tend to be near busy roads; one EPA study found the concentration of ultrafine particles in Los Angeles to be 25 times greater near freeways than in the rest of the city.
Because pollution falls hardest near road traffic and crowded urban areas, people who are more likely to live there — the poor, the elderly, people of color — are disproportionately exposed to airborne neurotoxins. In 2014, researchers from the University of Minnesota found that minorities in the United States are exposed on average to 38 percent higher levels of air pollution than white people. (Though they looked at nitrogen dioxide, a nonparticle pollutant, their findings are indicative of traffic-related exposures.) In 2012, researchers from Yale matched census tracts to particle pollution data for areas around the continental United States. They found that “non-Hispanic blacks, the least educated, the unemployed, and those in poverty” suffered the highest pollution burden.
The good news is that air pollution is one of the United States’ greatest environmental success stories. Particle emissions have been dropping steadily since the 1970s, along with other pollutants governed by laws like the Clean Air Act. The EPA regulates levels of coarse- and fine-particle pollution, and two years ago it strengthened the national standards for fine particles. But there is still no regulation for ultrafine-particle pollution, here or in any other country. While the EPA did consider the new science implicating ultrafine particles in brain disease during its last review, an agency representative told me by email that there was “insufficient evidence to draw conclusions.” The agency has said that it will consider the new science on ultrafine particles in its current review, which is ongoing.
The quickest way to rid our cities of particle pollution would be by cleaning up diesel engines. That may be in the works; the Obama administration recently proposed much tougher emissions standards for trucks. Since 2007, the EPA has required new diesel buses and trucks to utilize cleaner-burning engines, but because diesel engines last 20 or 30 years, millions of the older ones are still on the roads. Beginning around 2000, California started requiring owners of old diesel vehicles — from Greyhounds to big rigs and school buses — to begin replacing their engines. But a significant number of old, dirty engines are still on the road — and in many parts of the United States, engine upgrades are not yet mandatory.
Another option to reduce exposure is to move away from hot spots. But as Columbia University epidemiologist Shakira Suglia points out, because the risk tends to be highest in poorer neighborhoods, the people with the worst exposures “simply don’t have the resources to move. The less you have, the harder it is to control what it is you are being exposed to.” Some public health advocates’ suggestions for people who can’t move — like telling them to stay indoors on the worst pollution days — can seem impractical, even cruel. Broader efforts, like limiting vehicle traffic through neighborhoods and building schools and nursing homes far from busy roads, could offer a measure of relief, as could the installation of expensive air filters. (A California law requires new schools to be built away from freeways or equipped with filters, but there are major loopholes. Meaningful improvement may be decades away even in places like Los Angeles — not to mention developing megacities like Beijing and New Delhi.)
Meanwhile, it’s worth noting that those who study brain disease and air pollution are taking matters into their own hands. Every time she moves to a new place, Weuve says she aims to live “at least 50 meters away from an interstate expressway, state highway, or truck route.” When USC’s Finch moved to Los Angeles, he “chose to live at as high an altitude as possible” in order to escape the pollution that clusters around the city’s low-lying highways. Last year, before their daughter was born, MIT’s Cross and his wife began looking for a new home for their young family. “Minimizing her exposure to roadside emissions is something that played into our decisions,” Cross says. For any potential home, proximity to a busy road “was a deal-breaker.”
This story was supported by a Middlebury College Fellowship in Environmental Journalism.