Climate Connections is a collaboration between Grist and the Associated Press that explores how a changing climate is accelerating the spread of infectious diseases around the world, and how mitigation efforts demand a collective, global response. Read more here.
In early 2022, nearly 200,000 Malawians were displaced after two tropical storms struck the southeastern part of Africa barely a month apart. Sixty-four people died. Amid an already-heavy rainy season, the storms Ana and Gombe caused tremendous devastation across southern Malawi to homes, crops, and infrastructure.
“That March, we started to see cholera, which is usually endemic in Malawi, becoming an outbreak,” said Gerrit Maritz, a deputy representative for health programs in Malawi for the United Nations Children’s Fund. Cholera typically affects the country during the rainy season, from December to March, during which time it remains contained around Lake Malawi in the south and results in about 100 deaths each year.
The 2022 outbreak showed a different pattern — cholera spread throughout the dry season and by August had moved into Malawi’s northern and central regions. By early February of this year, cases had peaked at 700 per day with a fatality rate of 3.3 percent, three times higher than the typical rate. When cases finally began to decline in March, cholera had claimed over 1,600 lives in a 12-month period — the biggest outbreak in the country’s history.
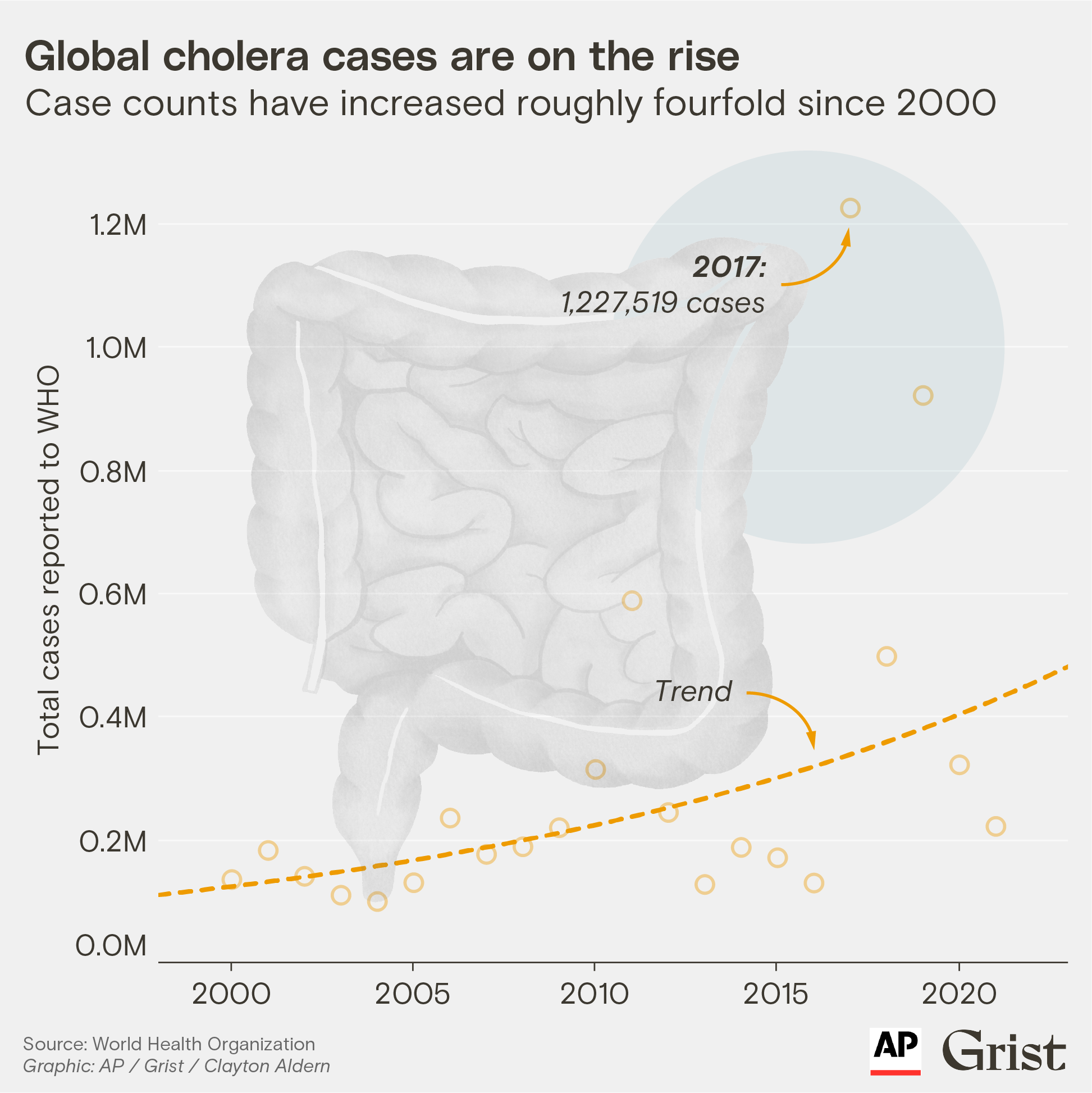
As climate change intensifies, storms like Ana and Gombe are becoming more frequent, more powerful, and wetter. The World Health Organization, or WHO, says that while poverty and conflict remain enduring drivers for cholera around the world, climate change is aggravating the acute global upsurge of the disease that began in 2021. According to WHO, 30 countries reported outbreaks in 2022, 50 percent more than previous years’ average; many of those outbreaks were compounded by tropical cyclones and their ensuing displacement.
“It’s difficult to say that [Tropical Storm Ana and Cyclone Gombe] caused the cholera outbreak,” UNICEF public health emergency specialist Raoul Kamadjeu said. “What we can say is they were risk multipliers.”
Cholera is a diarrheal illness that spreads in places without access to clean water and sanitation, when people swallow food or water contaminated with Vibrio cholerae bacteria.
“Malawi’s water-sanitation indicators were already extremely bad,” said Kamadje, “but the storms made a bad situation worse.”
Flash floods spread sewage into lakes and boreholes, washed away pipelines and sanitation infrastructure, and ruined roads integral to the delivery of supplies. By one government estimate, Ana alone destroyed 54,000 latrines and about 340 wells. People displaced from their homes turned to whatever water sources were available, often ones that were highly contaminated, and transmitted the disease as they moved to new areas.
While Malawi’s outbreak was spreading across its borders to Zambia and Mozambique, hundreds of thousands of people in Pakistan reported cholera symptoms amid a massive monsoon season that left a third of the country fully underwater. And in Nigeria, cases spiked after over a million people were displaced by extreme flooding during the 2022 rainy season.
The global cholera surge drove a vaccine shortage right when countries needed it most. Malawi in the past used the cholera vaccine for prevention, but “now if you don’t have an outbreak, you don’t get the vaccine,” said Otim Patrick Ramadan, WHO incident manager for regional cholera response in Africa. In response to the shortage, the international coordinating group for cholera vaccines changed its vaccination protocol in October from two doses to one, reducing protection from two years to about five months.
Climate change doesn’t only affect cholera through worsening floods and storms. Hotter temperatures and longer and drier droughts can also have an impact.
“With a severe shortage of water, the remaining sources become easily contaminated, because everyone is using them for everything,” Ramadan said. “We have seen that in the greater Horn of Africa.” Amid a prolonged and extreme drought, which has been directly attributed to climate change, Ethiopia, Somalia, and Kenya all saw cholera proliferate over the past year. In drought areas that have experienced crop failure, malnourishment has also reduced immunity to diseases.
Climate change doesn’t only affect cholera through worsening floods and storms. Hotter temperatures and longer and drier droughts can also have an impact.
Johns Hopkins University infectious disease epidemiologist Andrew Azman, who specializes in cholera research, cautions against making sweeping statements about climate change turbocharging cholera globally.
“We know cholera is seasonal in much of the world, but the associations between precipitation, drought, floods, and cholera are not really clear,” Azman said. “In some places, more precipitation increases cholera risk. In some places, it’s less precipitation.” He added that destructive storms in the past have not led to massive cholera outbreaks at the scale of the recent epidemic in Malawi, so it’s important to also consider other factors.
“While the storms may have created good conditions for transmission, the outbreak happened after a few years of relative calm in terms of exposures,” Azman said. “Immunologically, you had a much more naive population.” The strain circulating had also been newly introduced from Asia, and scientists are currently studying whether it was more transmissible.
Research suggesting that cholera is largely contracted from bacteria that lives in the aquatic environment and thrives under increasing temperatures has mostly been discredited, said Azman. “But one of the big mechanisms by which extreme events will impact cholera risk is the destruction of water and sanitation infrastructure,” he said. “That is an important point, because we can block those impacts if we invest in [those things].”
Climate Connections: A warming planet, pathogens, and diseases
Kamadju agrees. “Cholera is just a mark of inequity and poverty,” he said. “It’s a problem of investment, development, and infrastructure.” Malawi’s outbreak came at a time of economic crisis, with its currency devalued in May 2022. Limited health resources were also stretched thin by COVID-19 and a polio outbreak, the first in 30 years.
This March, a year after the cholera outbreak began and as cases were beginning to go down, Malawi and its neighbors braced for a new storm. Cyclone Freddy turned out to be the longest-lasting cyclone ever on record, causing untold damage and killing more than 800 people across Mozambique, Madagascar, and Malawi, with some counts even higher. But while cholera cases started to spike in Mozambique as predicted, in Malawi they continued their downward trend.
Ramadan says that’s in large part because the ongoing cholera response already occurring in Malawi’s southern region — high vaccination rates, advanced distribution of water tablets and supplies, and messaging around cholera — reduced transmission in spite of the direct impacts to infrastructure.
Maritz of UNICEF worries that a shift in Malawi’s methodology for reporting cholera cases may be giving a false impression of just how successful those mitigation efforts are. On June 1, as cases continued to decline significantly, Malawi shifted to an endemic protocol for measuring cholera, which requires a rapid diagnostic test and a lab sample to confirm an infection. In contrast, during an outbreak, anyone who presents at a clinic with symptoms gets marked as a case.
Kamadjeu said this strategy made sense given the low number of current cases. But Maritz says that capacity challenges and delays in testing with the new protocol have led to underreporting of cases.
[Read next: Mosquitos are moving to higher elevations — and so is malaria]
“We are still seeing people arriving at clinics with cholera symptoms that are not being reported in the national dashboards,” said Mira Khadka, an emergency health specialist leading cholera response for UNICEF in Malawi’s Blantyre district. It’s hard to mask a big cholera outbreak if people start dying, but the reporting lag is still cause for concern.
“Agencies that were responding to the cholera outbreak are now withdrawing,” said Khadka. “This can create the potential for another big outbreak to start.”
A team of government officials and health experts is assessing reporting methods in the southern districts where cases persist.
“What climate change means for us as a humanitarian agency is that we cannot do business as usual anymore,” Maritz said. “We are already preparing that most likely come January, February, there will be another cyclone with a huge flooding event.”