Dear Umbra,
I am eligible for the COVID-19 vaccine and my doctor has contacted me about an upcoming appointment. But I feel like others in more polluted communities could use it more than me. Should I get it or wait?
— Self-Hating Over Terrible System
Dear SHOTS,
Vaccine guilt is certainly the newest symptom to arise in the year-long psychodrama that is the COVID-19 pandemic. Before you even get to the ethical quandaries of worthiness, determining one’s own vaccine eligibility status is a challenge in its own right. Every state has a disparate and often Byzantine system to decide which groups should have priority over others, and those lists are updated and modified seemingly every other week! Twenty-something-year-old smokers in one state may have no trouble getting a vaccine appointment while in another, seniors with severe asthma are still waiting for a call from their doctor.
COVID-19 vaccine eligibility, as it turns out, isn’t much of a meritocracy. Add to that the fact that privileged groups — those with faster internet access and familiarity, more powerful social connections, and more free time — can more easily navigate the system of appointments, and you have a recipe for public health injustice.
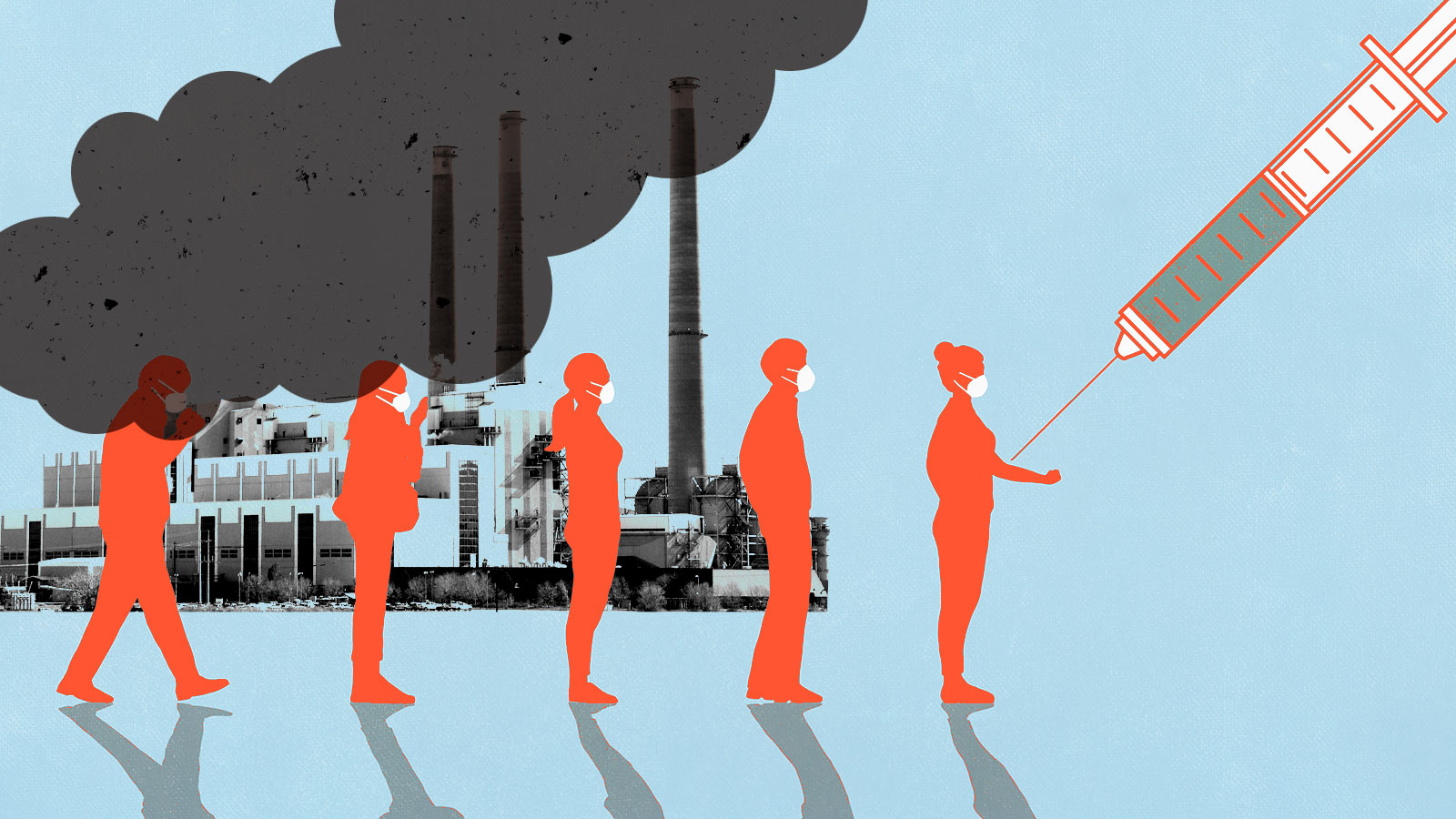
The cruelest reality of the vaccine system is that it is exactly those who are likely to struggle to get a COVID-19 vaccine appointment who need the shot the most! That includes people of color, service workers, the elderly, and the disabled. And to your point, those demographic groups are more likely to live in heavily polluted communities. Exposure to air pollution has been shown to be a significant risk factor for more severe COVID-19 outcomes. And yet, those burdened neighborhoods have been shunted aside in the vaccine rollout in places like Chicago.
You, SHOTS, have found yourself in a much-coveted position: You can access the vaccine in every sense of the word. There is a whole world of advice already out there about whether or not a person should take a vaccine when offered one, and the answer from medical professionals seems to be a resounding “yes, please, take it!” The larger goal of vaccinations is to create herd immunity, so the more people who can no longer act as disease vectors, the better.
And yet! Not every vaccination story screams “public health triumph.” Personally, any time I hear about someone who rushed to a clinic after hours to grab an extra dose they found out about via a friend of a friend, I think: Wasn’t there anyone you could have called who might need it more? Because while herd immunity is certainly the end goal, protecting those who have a higher risk of death by virtue of their jobs, health issues, or surrounding environment is a more urgent need. This dilemma will (hopefully) fade as more and more extremely vulnerable people are vaccinated, but in the meantime, there’s certainly no small amount of self-flagellation associated with getting a spot ahead of others in the lengthy vaccine line.
And yet the logistics of your particular situation limit your options. If you make an appointment for yourself to get a vaccine and pull a switcheroo at the last minute with a friend, family member, or even acquaintance who you feel needs it more, your intended good deed would likely yield a host of complications for the proffering hospital, clinic, or health department. Your decision could just end up being counterproductive for the vaccine distribution process. And the workers in that system are under extreme duress as it is!
You want to know what to do about your individual vaccine appointment, but that might be the wrong question to ask if your concern is really about environmental and epidemiological injustice. Perhaps we should start with why air pollution isn’t one of the factors that qualifies you to get a vaccine despite the fact that compromised lungs tend to make you more susceptible to respiratory illness. If you can claim to have smoked 100 cigarettes in your lifetime, for example, you will currently find yourself in a vaccine priority group in Pennsylvania, North Carolina, and a handful of other states — because, yes, being a smoker makes you more susceptible to COVID-19.
Why ask people to count every drunken Marlboro of their existence rather than their distance from the nearest coal-burning power plant or major freeway? Well, determining someone’s exposure to air pollution is a far more complicated thing to figure out, said Russell Zerbo, an advocate with the Clean Air Council in Philadelphia. “How would you even begin to put that in an evaluation to figure out someone’s need?” Zerbo asked. “How deep are you going to go into someone’s life in terms of questionnaires, and is it at the front of their mind that they live next to this demolition site or other possible source of air pollution?”
Not that it’s a bad idea — just difficult to execute. Zerbo said it would be “pretty radical, in a good way” to include questions in the eligibility questionnaires that address what kind of a neighborhood you live in, what kind of pollution sources are nearby, what the condition of the inside of your home is. (Because, not to fearmonger, but there are many potent sources of air pollution, even inside your very own kitchen!)
Air quality itself is something that is famously variable in how it’s measured and shared with the community. It can vary pretty significantly across even city blocks, and is affected by so many different forms of contamination, be it particulate matter or toxic chemicals or a combo platter of both, which is the specialty of my home of Allegheny County. But that said, it’s no secret that some neighborhoods and towns have far more documented sources of air pollution. It’s no secret where the industrial facilities, trash incinerators, and shipping warehouses in your city are located. Even the Environmental Protection Agency has an interactive tool where you can get a pretty good sense of your area’s pollution burden.
And certain areas have tried to take neighborhood factors into their COVID-19 vaccine rollout. In Dallas County, Texas, officials actually attempted to prioritize certain ZIP codes so that all residents of these poorer, more racially diverse, and heavily polluted areas would be eligible. But then the state government shot that down idea, threatening to reduce their vaccine allocation unless they returned to the standard age-based system.
I posed your specific vaccine question to Sherri Mixon, the director of the T.R. Hoover Community Development Center in South Dallas, who is working with a group of local stakeholders to get the less computer-savvy residents of the area vaccinated.
“I’d tell that reader to not feel guilty,” she said, “But I’m gonna tell that reader also: Now that you are aware of the disparity, use your voice, use your skill, get out there and help those communities, because when you help them, you also help your city as a whole. We can’t get back to our regular way of life until we are all vaccinated. And it’s gonna take people that are vaccinated to go back and work in these communities to help others become vaccinated.”
The guilt you are feeling over your level of privilege does not in and of itself help those who are less fortunate. COVID-19 is a dire threat and has caused untold damage — physical, economic, psychological — in the past year, but the disparities in death rates and vaccine distribution are expressions of the racial and socioeconomic inequities that have permeated American society for generations. Once the pandemic ends, those injustices still have to be dealt with!
For example, I talked to 76-year-old activist and former U.S. Steel employee Art Thomas, who has lived in the Western Pennsylvania town of Clairton almost his entire life. Clairtonians breathe some of the most toxic air in the entire country, courtesy of one of the very few remaining steel mills in the region that continues to operate there, and the town has extremely high rates of both cancer risk and poverty. Here’s what Thomas said to me:
“I believe Clairton air is killing more people here than all the violence and coronavirus and everything else. Personally, I don’t know anyone in the city of Clairton that died from COVID. If you want to get into people with cancers, pulmonary diseases, sleeping with CPACs and stuff like that, I know a whole bunch of them. I wear a mask, I wash my hands, I keep my distance, I don’t go to Trump rallies, so I think I’ll survive the COVID. But I gotta breathe every day the stuff they’re putting in the air, so I’m more scared of the Clairton mill.”
There are plenty of opportunities for vaccinated individuals to give back right now: You could volunteer with the local health department, for example, which can probably use extra hands doing administrative work for clinics. But what about after the pandemic? I urge you not to abandon your concerns for those polluted communities. Do some research into civic engagement opportunities. What meetings and votes can you show up to? What organizations can you volunteer for? Offer to help wherever you can, while being careful not to assume you know what’s best.
One day we won’t have to be afraid of every cough within a 1-mile radius, and that will be an excellent day indeed! But it won’t mean that every threat to marginalized or vulnerable people has been abolished. There’s still work to be done.
In good health,
Umbra