If you plan to have sex anytime soon, let’s hope it’s not in Niger, Africa.
According to the nonprofit organization Save the Children, just 4 percent of couples in Niger have access to birth control. Although the situation in this West African country is extreme, more than 125 million couples worldwide — most of them in developing countries — cannot get contraceptives. Some of the children that have resulted from these couplings were wanted and some were not, but one thing is certain: Lack of access to birth control increases the burden on already strained parents and on the global ecosystem.

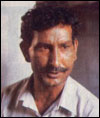
Sujoy Guha (right), with Ronald Weiss.
Sujoy Guha, professor of biomedical engineering at the Indian Institute of Technology in Delhi, believes he has the answer to this problem. Highly regarded in India for his work on everything from disability rights to drinking-water purification, Guha has spent the last 25 years perfecting his invention, Reversible Inhibition of Sperm Under Guidance, better known (thankfully) as RISUG. RISUG, he says, has all the advantages of the perfect contraceptive — and, some would say, a surprising bonus: It’s made for men.
RISUG works by an injection into the vas, the vessel that serves as the exit ramp for sperm. The injection coats the vas with a clear polymer gel that has a negative and positive electric charge. Sperm cells also have a charge, so the differential charge from the gel ruptures the cell membrane as it passes through the vas, stopping the sperm in their tracks before they can even start their journey to the egg. RISUG doesn’t affect the surrounding tissues because they have no charge.
Compared to the other male contraceptive choices currently available — abstinence, withdrawal, condoms, and vasectomies — RISUG is a whole new ballgame. In fact, Guha and others believe, the contraceptive promises to be even better than the choices available to women. Guha enumerates six advantages of his invention:
- First, neither sexual partner has to interrupt the throes of passion to use it — no more running to the bathroom and fumbling with various ointments and plastics.
- Second, the process, once it is refined and approved, will be completely non-surgical. Whew, say a lot of men.
- Third, it’s long-lasting. According to Guha, a single injection can be effective for at least 10 years.
- Fourth, after testing RISUG on more than 250 volunteers, neither Guha nor other researchers in the field have found side effects more worrisome than a slight scrotal swelling in some men immediately following the injection. This swelling goes away after a few weeks. Compare that to the Pill, which even today can cause health problems ranging from severe migraines to blood clots.*
- Fifth, it works. Of all the men who’ve had the RISUG injection (and 15 of the 250 had it more than 10 years ago), there has been only one unplanned pregnancy among their partners — and in that instance, the injection wasn’t administered properly.
- Sixth, and best of all, the contraceptive appears to be reversible with another injection. To date, reversing the procedure has been tried only on non-human primates, but among them, it’s been reversed successfully multiple times.
A RISUG volunteer
after more than
10 years of
testing.
If RISUG’s current stage of clinical testing goes well, it will be on the market in India by next year. Within a few more years, if all proceeds as planned, the injection to reverse it will also be on the market.
Just Shoot Me!
But would men in India — or anywhere else — use it? Every U.S. male authority I talked to in the field, including experts at the World Health Organization and the U.S. Agency for International Development, pooh-poohed the idea. “Men don’t like doctors to have anything to do with their testicles,” summarized Don Waller, a contraceptives expert and professor of pharmacology and toxicology at the University of Illinois at Chicago.

Condoms are so 20th century
when it comes to birth control.
Maybe not — but one in six married men in the U.S. have had vasectomies, which definitely require medical personnel poking at the gonads. Moreover, surveys conducted by the University of Edinburgh, the Kaiser Foundation, and other entities have shown that in countries as diverse as Hong Kong, South Africa, and the U.S., the majority of men say they want more options for male contraceptives.
But even if men used RISUG, would women trust them? It’s doubtful that the whispered promise of having been RISUGed would fly during a one-night stand. However, in the context of a committed relationship, RISUG could shift some of the responsibility for family planning off the women who have borne (and born) too much of it for too long, at the expense of their health, time, finances, and emotions.
That shift is definitely possible, according to Ronald Weiss, a vasectomy specialist in Ottawa*, who says men’s attitudes toward contraception are changing. “In Canada, 10 years ago, it used to be tubal ligations [the more-invasive female equivalent of a vasectomy] to vasectomies were performed at a ratio of 2 to 1. Now that number is reversed.” Weiss believes a lot of men would prefer a procedure that wasn’t permanent. And, he says, RISUG is the most promising male contraceptive out there.

A bitter Pill to swallow?
Still, there’s been a lot more media fervor over the possibility of a male version of the Pill — even though its potential side effects for men include everything from liver damage and prostate problems to what is referred to in the literature as gynecomastia. Translation: Men growing breasts.
Weiss thinks RISUG is preferable. “The only people who should be excited about the male Pill are pharmaceutical companies,” he said. He believes so much money has been poured into researching the Pill because pharmaceutical companies want something consumers will have to buy again and again — as opposed to an inexpensive, one-time injection. In the U.S., a decade of the female Pill costs about $3,600. RISUG would be dramatically less expensive, while pharmaceutical companies would have to pay $25 million to $40 million to bring it to market.
But from the consumers’ point of view, RISUG could be a godsend during the approximately 30 years the average person spends trying not to cause a pregnancy. It would mean fewer women getting cancer from the Pill or having their uteruses perforated by an errant IUD. It would mean fewer men having to choose between the risk of a burst condom or the permanence of a vasectomy.
And in the developing world, RISUG would mean much more.
This Little Injection Went to Market …
“Realize that overseas there just aren’t decent options,” said Elaine Lissner, director of the Male Contraception Information Project. “By the time condoms arrive there, they’re cracked by the heat. Poverty and lack of medical follow-up are a problem. You can’t use a diaphragm if you don’t have clean running water. You can’t use an IUD if no medical treatment exists if something goes wrong. You can’t use the Pill if it’s too expensive.”
In the developing world, RISUG’s price tag could be brought down to about $22, the price at which Guha and Indian Drugs & Pharmaceuticals Ltd. (the largest Indian drug company) are planning to market it in India. This makes RISUG potentially affordable by even the world’s poorest.
Studies have shown that when couples in the developing world start having fewer children, both the health and literacy of the children improve, and mothers are more likely to survive long enough to raise their kids. Moreover, families with fewer children have less impact on the natural world, because they are not as desperate for firewood, water, and bush meat.
This “less children/healthier environment” connection has become so clear that wildlife organizations have started to team up with family-planning groups in biodiversity-rich areas of the world. In the Montes Azules Biosphere Reserve in Mexico, Conservation International is working with Mexfam to slow the clearing of the forests as well as to offer people there the option of reproductive health care.

A nurse prepares to distribute condoms.
Photo: USAID.
Inevitability, talk of providing contraceptives to people in developing countries raises allegations of racism — but there’s a huge difference between forced eugenics and offering people the choice to control their own fertility. According to Save the Children, 72 percent of Sweden’s population has access to contraceptives; why shouldn’t the same choices be available in Niger? With the world’s population growing by 77 million people per year, access to contraceptives is not something the industrialized world can continue to hog.
So far, what’s holding up the potential marketing of RISUG outside of India is safety testing. Although the Indian medical community maintains that its safety testing is better than that of the U.S., Jeff Spieler, chief of research at USAID’s Office of Population and Reproductive Health, said, “The pre-clinical toxicology testing in India [on RISUG] was weak.”
Lissner agreed that some of the older studies should be redone, but given the near-perfect record of RISUG so far, she noted, “If I were a man, I’d feel safer having RISUG injected than eating non-organic fruit.”
RISUG will probably soon be marketed in India, but the U.S. will play a critical role in determining its use elsewhere in the developing world. Grants from U.S. agencies, corporations, and nonprofits spur on a significant portion of the world’s research. But, said Waller of the University of Illinois, “If funds from the U.S. are paying for another country’s research, then the research has to be already approved by the FDA. Otherwise it looks like we’re using the rest of the world as experimental subjects.” Thus, lack of interest in RISUG by the U.S. helps delay its use around the world.
Meanwhile the developing world waits.
As Lissner said, “Every month we delay means thousands more women dying in childbirth, more families in poverty from too many children, and more women dying in attempted abortions.”
*[Correction, 14 Aug 2003: This article originally stated that birth control pills can cause ovarian cancer. In fact, studies show that the Pill can protect women against ovarian cancer.]
*[Correction, 18 Aug 2003: This article originally stated Ronald Weiss is based in Toronto. He is based in Ottawa.]