Climate Connections is a collaboration between Grist and the Associated Press that explores how a changing climate is accelerating the spread of infectious diseases around the world, and how mitigation efforts demand a collective, global response. Read more here.
In the 1990s, two hurricanes devastated Samoa in the South Pacific Ocean, wiping entire communities off the map and killing dozens of people. “Everything was just decimated,” Malama Tafuna’i, a primary care physician in Apia, the territory’s capital, said. “It looked like a bomb had gone off.”
A young girl at the time, Tafuna’i watched as her father, a doctor, would go out to treat patients while her household navigated the aftermath of the storms.
“He still had to go to work and the rest of us had to figure out, you know, how do we make sure that we’ve got a shelter for tonight or where are we going to get food from?’” she said.
Tafuna’i’s early experiences help her navigate the impacts of climate change, both as a physician and as a citizen of Samoa, where extreme weather events frequently upend daily life. She uses the knowledge she has accumulated to help other doctors consider climate impacts when treating patients.
Tafuna’i, who has practiced medicine in Samoa for the better part of two decades, knows that once the hurricane-force winds die down and the flood waters recede, public health disasters — vector-borne disease outbreaks, bacterial infections, malnutrition due to crop loss — soon follow. People lose their homes in these storms and spend days exposed to mosquitoes and other pathogen-carrying insects. Decaying sanitation systems overflow and spread E. coli and other dangerous bacteria through communities. Entire fields of crops are wiped out by flooding, and families already struggling with food insecurity go hungry.
Tafuna’i can spot these links between extreme weather events and disease, but actually treating the effects of rising temperatures on the Samoan population can be tricky. It’s exceedingly difficult to assess a sick patient and determine that climate change itself is the main driver of that patient’s illness, Tafuna’i said. What she does see, however, is that climate change compounds and exacerbates existing health inequities in Samoa.
“Once a disaster hits, it sets back the whole system big time,” said Tafuna’i, adding that then “we have to figure out a way back up to wherever the starting point was at the time.”
As the planet warms, Samoans and millions of other people around the globe will increasingly see their health affected by warming. Climate change, the World Health Organization says, is the “single biggest health threat facing humanity.”
Climate-driven malnutrition, malaria, diarrhea, and heat stress are projected to kill an additional 250,000 people worldwide every year, which will come with an annual cost of between $2 and $4 billion. And those are just a few of the leading causes of climate-related mortality. There are countless other ways in which our changing planet affects human health, some of them still beyond our understanding.
Samoa only has two hospitals, one of which is a 20-bed facility staffed by junior doctors. Ten health clinics staffed primarily by nurses serve Samoa’s rural population. The Samoan medical system, severely underfunded and understaffed, is far less prepared to shoulder the burden of rising temperatures than developed countries in the West. Nevertheless, doctors like Tafuna’i, who have long worked on the front lines of the crisis, have been among the first in the world to recognize the importance of arming doctors with the tools they need to both recognize how climate change will affect human health and to properly treat patients experiencing the health ramifications of a rapidly changing environment.
For many years, Tafuna’i was the only clinical lecturer at the National University of Samoa, a tiny medical school on the island of Upolu. She noticed that the school wasn’t teaching students about climate change — an omnipresent issue on an island that is experiencing some of the most severe sea-level rise on the planet.
[Read next: Climate change may be fueling a global surge in cholera outbreaks]
“You can definitely see that climate change has a huge impact on health, but it wasn’t in our curriculum at the time, and it wasn’t something we spoke about,” Tafuna’i said. So she invited colleagues from other universities, along with climate and related experts, to come speak to her students about the crisis. She also developed a climate-and-health curriculum that sent fourth-year students into remote parts of the island to analyze how climate change affects the well-being of rural communities.
In recent years, as rising temperatures have triggered public health emergencies of growing magnitude all over the globe, medical professionals and research institutions in the West have begun to catch on.
Renee Salas, a doctor at Massachusetts General Hospital in Boston, remembers a time climate change walked into her emergency room. It was 2019, and Boston was in the throes of a record-breaking heat wave. A team of emergency medical technicians arrived in an ambulance carrying an elderly gentleman suffering from heatstroke, the deadliest form of heat-related illness. The patient’s rectal temperature was 106 degrees Fahrenheit, which meant death was imminent. The emergency workers told Salas that when they climbed up the stairs and opened the door to the man’s apartment, it felt like they were being “hit with heat from the Sahara desert.” The patient and his wife, who both lived in the apartment, didn’t have air conditioning. Just one window was cracked open.
Salas and her team managed to save the man’s life, but the incident still weighs on her. “I often think about that patient’s wife who still remained in that same apartment,” she said. “We know from data that more than one-third of heat-related deaths are due to climate change, and that is making that disease more likely.”
A year after that incident, in 2020, the Lancet, a premier medical journal, published a frightening assessment of the latest research and data on the intersection of warming and health — its “most worrying” outlook since the journal began publishing the assessments in 2016. Almost every indicator of health tracked by the dozens of interdisciplinary researchers who compiled the report, such as excess morbidity and mortality, showed evidence of climate stress (extreme weather events, vector-borne disease, wildfire smoke, the list of stressors goes on). Two-thirds of the cities surveyed by the report said they “expected climate change to seriously compromise their public health assets and infrastructure.”
Salas, who had been reading the Lancet’s reports for years, saw that climate change was threatening “the very mission” of why she went into medicine in the first place. She decided to dedicate her career to the climate-and-health overlap. But at the time, no one in her circles was thinking about how climate change was going to affect medicine. In the United States, lawmakers were still arguing over whether climate change was even happening.
In the years since, however, Salas has seen a marked shift in the way the public, especially the medical community, thinks about climate change. “This has become mainstream medicine,” she said. Climate change has infiltrated the zeitgeist at hospitals across the U.S. for one key reason: “Fundamentally,” Salas said, “climate change makes our job harder as doctors.”
In the U.S., networks and groups such as ClimateRx, the Medical Society Consortium on Climate and Health, and Climate MD have cropped up with the aim to bring “climate solutions to the bedside.” Those efforts — which include teaching doctors how to recognize climate-related illnesses, such as tick-borne diseases and heatstroke, in patients and communicating about climate change with patients in a hospital setting — haven’t been immune to typical growing pains. The disparate initiatives within the larger climate-and-health movement are disorganized, and there’s no easy way for the various sects to share data and know-how. But that’s starting to change.
In May, the National Institutes of Health funded a first-of-its-kind national Research Coordination Center on Climate and Health, based jointly at Harvard and Boston University. The research center, described as a “clearinghouse to facilitate data exchange and share best practices,” provides a blueprint for what needs to happen on a global scale.
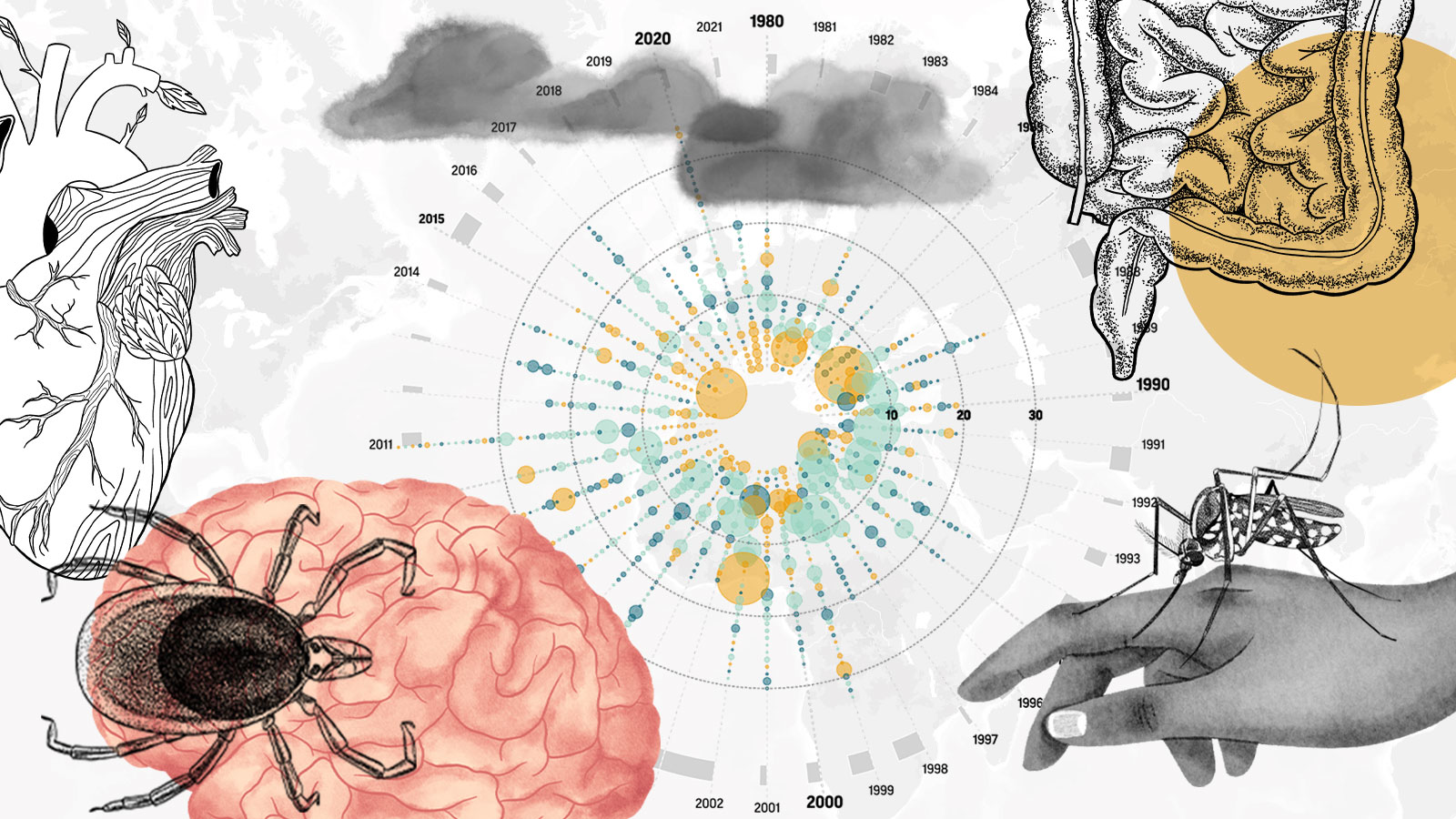
Climate Connections: A warming planet, pathogens, and diseases
Meanwhile, doctors like Tafuna’i are sitting on years of knowledge about global warming’s unbound potential to erode public health and stress health systems. Tafuna’i’s experiences teaching students and treating patients in Samoa could serve to inform and educate countries that are just beginning to confront these challenges. But, thus far, there’s been no indication that the West is looking to Samoa and other nations on the front lines of climate change for guidance.
“You can’t share your wisdom if you’re not at the table,” said Sheila Davis, chief executive officer at Partners In Health, an international public health nonprofit that helped devise a COVID-19 response in the U.S. based on prior efforts to eradicate HIV in Haiti and Ebola in Sierra Leone and Liberia. “Raising the voices of those who have the true expertise, it’s going to take all of us to push for that to happen.”
COVID-19 taught the world a valuable lesson: Pandemics can’t be defeated piecemeal. Studies indicate that the next pandemic may be fueled by climate change. The logical next step is to prepare — not individually, as siloed nations, but as a network of human beings around the world.
“How do you put a program in play that can be sustainable and then be something that’s shared?” Tafuna’i asked. “We have to decide what the priorities are for adapting to climate change.”