In January 2020, when the novel coronavirus was making its way across China, a woman eating at a restaurant in Guangzhou had the virus and didn’t know it yet. She infected nine of the 82 other people eating at the restaurant that day. Months later, researchers uncovered the reason why the infected diner got some people sick while others walked away unscathed: An air conditioning unit near the woman had carried the virus through the air, circulating it in a pattern through the restaurant.
Some 1,600 miles south of Guangzhou in Singapore, Stephen C. Schuster, director of the Singapore Center for Environmental Life Sciences Engineering at Nanyang Technological University, watched the research coming out of China with interest. It fascinated him that airflow, just as much as virology, seemed to be a critical factor in many early studies of how the virus worked. For years, his research has focused on something similar — not the way airflow affects coronaviruses, but the way ventilation affects the entire planet.
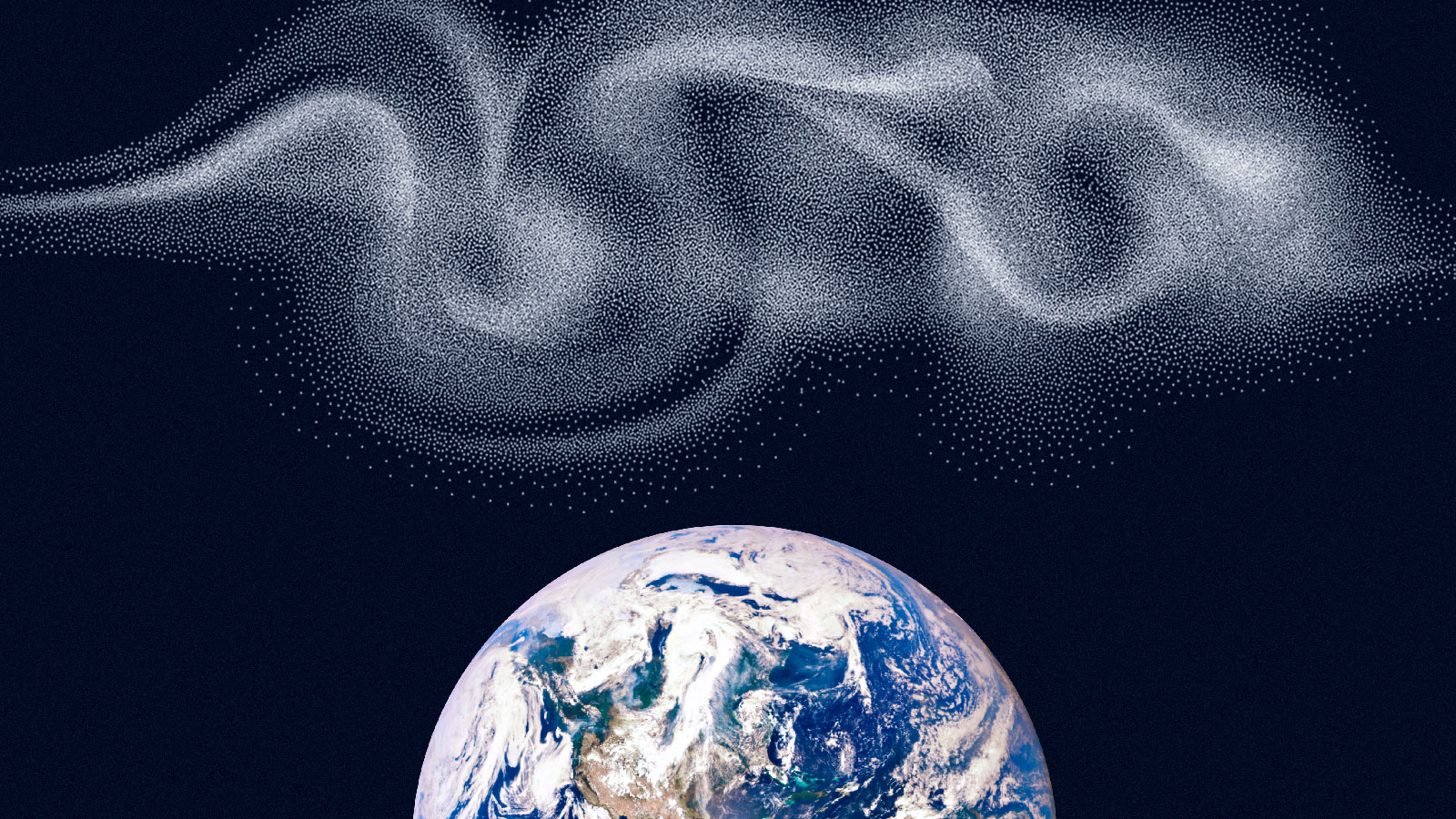
Last week, Schuster and a team of researchers in Singapore published a study shedding new light on the air microbiome — the puzzling and complicated combination of microorganisms in the air. If this is your first time hearing the term “air microbiome,” you’re not alone. Most researchers don’t even know it exists, Schuster said. But there is an entire ecosystem in the air, just like there are terrestrial and aquatic ecosystems teeming with life across the planet.
“People make the assumption that there’s nothing in the air because we can’t see it,” he said. But there is another world up there swirling with bacteria, fungi, and other microorganisms that have been blown off the surface of the planet and suspended in the air. Schuster’s study is the first in the world to examine how climate change may be affecting the way this invisible ecosystem moves. His paper cracks open the door to an entirely new chapter of research into the field of air microbiology and its implications for human and planetary health in a warming world.
Four years ago, Schuster set about trying to map the air microbiome and quickly ran into trouble. He set up air samplers on a building in Singapore called the Pinnacle@Duxton, the tallest public residential complex in the world, and found the exact same combination of fungi and bacteria in the air on the ground floor as he found on the 50th floor. He sampled air at the bottom of a mountain in Switzerland and turned up the same formula of bioaerosols as there were at the mountain’s peak. How could it be, he wondered, that there was absolutely no change to the air microbiome no matter how high up in the sky you went? He knew he was doing something wrong, but what was it? “There were so many months and years where I thought, ‘Oh my god, I’m going to fail,’” he said.
The problems Schuster ran into with his research echoed the crux of the analysis of that COVID-infected diner in Guangzhou. Schuster wasn’t accounting for ventilation and airflow. He didn’t realize that the air he was measuring at the bottom of the mountain was flowing up along the ridge to the top of the peak, so the air he sampled at the top of the mountain was the same air he had tested just minutes earlier below. And he also wasn’t accounting for a phenomenon called “atmospheric mixing,” when warm temperatures and turbulence mix up all the microorganisms in the air like a giant centrifuge. Peak mixing occurs during the day, when temperatures are warmer, and settles down at night, when it gets cooler.
Once he had developed a system for analyzing the air column that accounted for airflow, using sensor technology climate scientists have been using for years, Schuster and his team hit the jackpot. They were able to create a vertical map of the atmospheric microorganisms in the lower atmosphere, between 300 and 3,500 meters off the ground. By running many tests on the concentrations of atmospheric microorganisms at different heights and at different times of the day and night, Schuster’s team found that the factor that determines how those microorganisms are distributed and move through the air is temperature. “That’s the climate connection,” Schuster said.
Warmer temperatures change the formula of fungi and bacteria in the atmosphere. More warming equals more fungi, many of which are pathogens, rising up through the earth’s boundary layer — the lowest part of the troposphere. “With climate change, the fungi are now being transported to a higher and higher level” within the troposphere, Schuster explained. The higher fungi rise off the ground, the more easily they can spread out and colonize new terrain. “At the moment you are at a high level, you can distribute much much wider,” he said. In the tropical regions of the world, the air microbiome has a lot more fungal pathogens, plant pathogens, and bacteria swirling around than the air in colder regions.
The takeaway is alarming: As the planet warms, Schuster’s research suggests that those tropical air microbiomes could move north and south. Eventually, they might even reach the Earth’s poles, Schuster said. “This will mean that plant and animal pathogens will become invasive in regions where they are currently not seen,” he added. That could have implications for humans and the crops we grow for food.
“The study was done very well,” Mary Ann Victoria Bruns, a professor of soil microbiology and biogeochemistry at Pennsylvania State University who was not involved in the research, told Grist. “What we really need to understand to a much greater extent is how microbes are responding to environmental factors that are highly driven by climate change.”
Ken Aho, an associate professor of community ecology and statistics at Idaho State University, agreed, calling Schuster’s paper “a big addition.”
Schuster doesn’t know what the knock-on effects of the higher and wider distribution of fungal pathogens may be on people or crops, but he suspects that humans who are immunocompromised are already experiencing the effects of climate change on the air microbiome. A previous study Schuster worked on, published in 2020, showed that people in Singapore are breathing in between 100,000 and one million species of microorganisms every day. He’s using that finding to try to figure out how those microorganisms might be affecting people with respiratory problems, such as asthma or chronic obstructive pulmonary disease. The research is still ongoing, but Schuster’s hypothesis is that people with chronic respiratory illnesses may be affected by the fungal pathogens in the microbiome, and may be poised to suffer worse symptoms as climate change accelerates.
Bruns warned that Schuster’s findings, while significant, don’t necessarily mean that the fungal pathogens and other microbes floating around in the air microbiome are all capable of causing illness in immunocompromised people. “Just because he discovered DNA doesn’t mean that these are live cells,” she said. “We don’t really know how infectious these particles are. But I think it’s reasonable to say yes, temperature is affecting the mix of microorganisms that we are all exposed to on a daily basis and we should probably expect higher risks of exposures to different pathogens.”
Schuster hopes his study will inspire researchers in other places around the world to use his system for sampling the air microbiome to map the air columns where they live and help him create a global map of the air microbiome. “We can be the doctors for this planet and the atmosphere by monitoring how this air microbiome composition will change in different climatic conditions,” he said.