The Centers for Disease Control and Prevention — the federal agency that monitors diseases and establishes guidelines to protect human health — published a paper last month that shows cases of Lyme disease jumped nearly 70 percent nationwide in 2022. But what looked like an alarming spike in disease was actually the result of smarter disease surveillance that better reflects what’s happening on the ground.
The CDC revised its Lyme reporting requirements in 2022, making it easier for states with high infection rates to report those cases. The report, the first published analysis of the new data collection guidelines, demonstrates the crucial role efficient surveillance plays in better understanding the scope of infectious disease in the U.S. — and what more must be done to safeguard public health as climate change fosters the proliferation of ticks.
“Disease surveillance that is interpretable and is standardized is integral to being able to understand how disease frequency is changing, and if it’s changing,” said Kiersten Kugeler, a CDC epidemiologist and lead author of the paper. She noted that climate change will complicate the already difficult task of monitoring and controlling diseases such as Lyme. Cases in some areas will continue rising, and they’ll decline in others, as parts of the U.S. become more amenable, or hostile, to ticks. “It’s not going to be straightforward,” Kugeler said. “It’s going to be incredibly important to have good surveillance to be able to understand how climate is affecting risk of disease.”

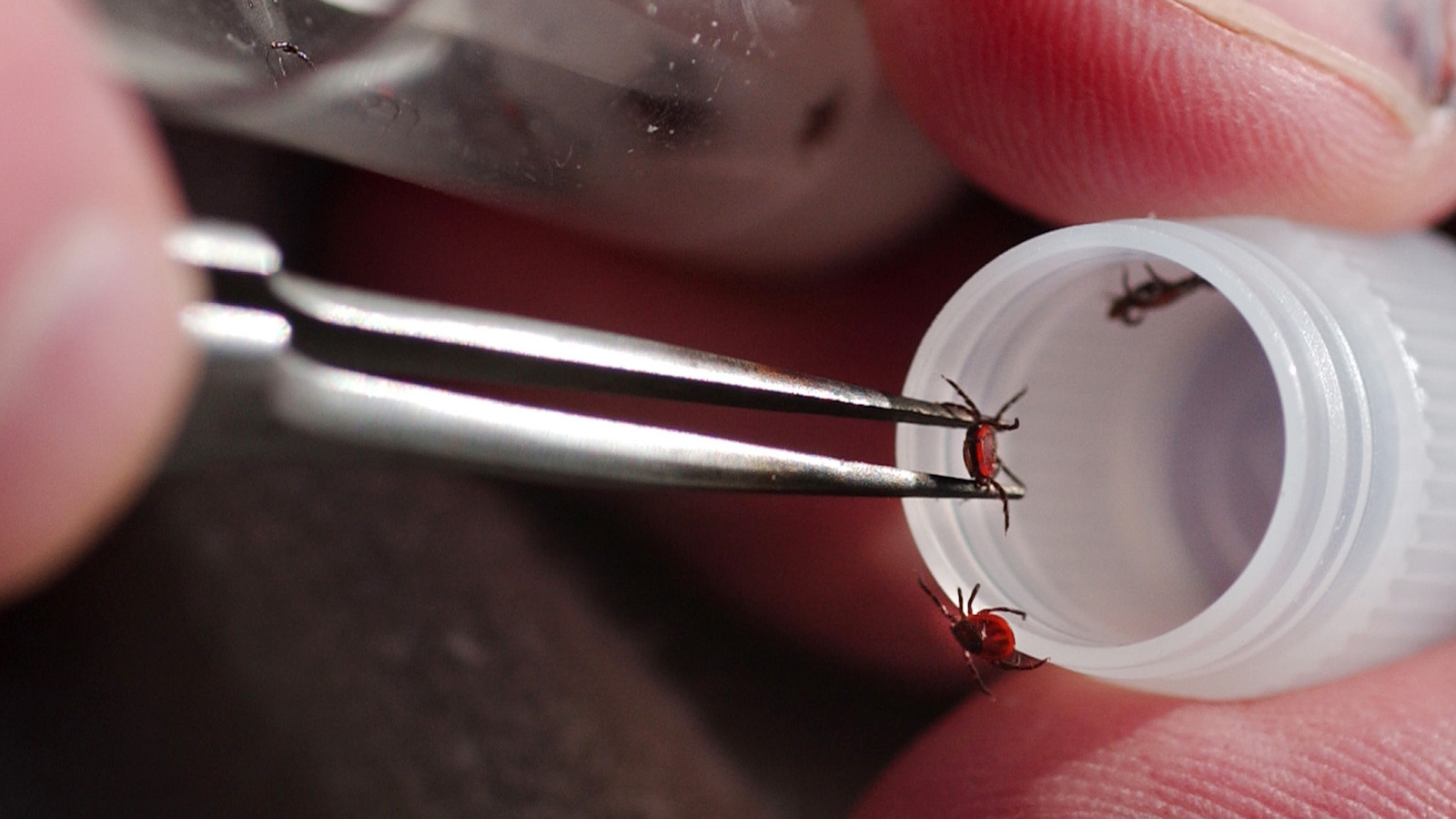
Studies have documented significant shifts in Lyme trends across the country. The illness is caused by the bite of a black-legged tick and causes symptoms that range from flu-like and mild to neurological and debilitating, depending on how quickly the disease is diagnosed. Cases doubled in the three decades between 1990 and 2020. Many researchers, including CDC employees, say climate change is one factor behind that precipitous rise. Environmental changes such as urban sprawl and swelling populations of white-tailed deer, among other drivers, also play a role.
Warmer winter temperatures have coaxed black-legged ticks into regions that have historically been too harsh for the blood-sucking arachnids. Meanwhile, milder spring and fall seasons have given the pests more time to breed. Lyme is a portent of climate-driven diseases to come. But, as it has spread into new areas and infected more people, the CDC has struggled to capture the full impact.
In 2022, the agency redoubled its disease surveillance efforts, with a special emphasis on vector-borne disease. As part of that push, the CDC loosened its Lyme disease reporting requirements in the Northeast, mid-Atlantic, and upper-Midwest, where cases are high. Public health departments in those areas no longer have to track down the clinical details of each positive Lyme test, such as a patient’s symptoms and when they began, and doctors can skip the labor-intensive process of recording and reporting them. Now, a positive laboratory test is sufficient. Eliminating these steps takes the onus off doctors and local public health authorities and puts it on state health departments, which are typically better equipped to handle it.
“We have a lot of behind-the-scenes data management that’s new with this Lyme disease surveillance system,” said Rebecca Osborn, a vector-borne disease epidemiologist at the Wisconsin Department of Health Services. But overall, she said, “It has gotten quite a bit less burdensome.”
The new system runs the risk of including information on people who no longer show symptoms but are still testing positive for the bacteria, which can linger in the blood for years after the infection has gone. But those cases likely comprise a small fraction of the overall data, the CDC said. In areas where Lyme remains rare, providers must continue reporting clinical information for each case.
These relatively modest changes to the case definition requirements unearthed 62,551 cases of Lyme nationwide. That’s 1.7 times the annual average reported from 2017 to 2019.

Still, most cases of Lyme disease in the U.S. go unreported. Studies based on health insurance records estimate that roughly 500,000 cases are diagnosed every year. Those reported by states to the CDC in 2022 comprise less than one-fifth of that. Elizabeth Schiffman, an epidemiologist with the Vector-Borne Diseases Unit at the Minnesota Department of Health, said figuring out how to capture every case is nearly impossible and perhaps beside the point.
“No system is ever perfect,” she said. “We’re always going to miss something, we’re always going to count something that probably shouldn’t be counted.” If the CDC could use the data it collects every year under its new system to measure the overall impact of Lyme, Schiffman said, then the number of cases it already knows about may be enough.
“If what we are able to capture is able to give us an idea of where things are happening, how things are changing, and inform good public health actions, then it could be argued that we don’t need to count every case.”
The data deficit and lack of standardization among states becomes more of a problem when researchers try to tease out the impacts of climate change on the disease. The CDC argues that in regions where Lyme incidence is still relatively rare, the updated surveillance system doesn’t make sense. Doctors and local health departments in those areas still need to collect clinical information on every potential Lyme patient, because each case is a revealing datapoint rather than a statistic in a larger trend. But the burdensome requirements in low-incidence areas muddy efforts to detect the role of climate change in how black-legged ticks may be migrating, said Richard Ostfeld, a senior scientist at the Cary Institute of Ecosystem Studies who researches tick-borne illnesses.

The prevalence of Lyme disease typically falls along geographic lines. Counties in the upper Midwest and Northeast report tens of thousands of cases each year, while those in the Southeast and South report hundreds. Although the CDC’s revised reporting guidelines more accurately revealed the extent of Lyme disease in areas with a high prevalence, the implementation of the system over time may obscure growth of the disease elsewhere. The new guidelines “would tend to bias your estimate of geographic trends toward more growth in incidence in northern parts of the country as opposed to southern parts of the country where you’re still being very conservative,” Ostfeld said. “It complicates matters for those trying to understand the role of climate change.”
North Carolina, for example, a state long classified as low-incidence, was among five states with the highest number of Lyme disease-related insurance claims in 2016, according to one analysis. But the disease reporting there, said Noah Johnston, director of the Lyme awareness group Project Lyme, still isn’t where it needs to be. “There’s an expectation that tick populations in North Carolina are not as high as they are in the Northeast,” he said.
The benefits and drawbacks of the CDC’s updated surveillance highlight the difficulties of tracking and controlling infectious diseases under climatic conditions that are rapidly shifting the distribution of disease carriers. Incremental adjustments to the status quo might not be enough to keep up with the growing scale of disease risk. “We’re likely going to see more and more cases of these diseases and more and more diseases that are going to affect not just our population in the U.S., but globally,” said Osborn. “Public health in general needs to become a little more proactive in our responses. We’re still working on that as a field.”